| THE PEOPLE VS. HMO'S | |
| September 30, 1999 |
||
|
|
Health correspondent Susan Dentzer reports on a 1997
Texas law that allows patients to sue managed care plans in state
court if they are denied medically necessary care. The Health Unit is a partnership with the Henry J. Kaiser Family Foundation. |
|
SPOKESMAN: We believe you can't sue your way to better health. SPOKESMAN: The people that they have harmed have a right to go to court.
ROSEMARY DUDLEY: I've never been lawsuit conscious, but when I get to thinking about this, I can ... I just get to feeling very bitter and vindictive, and think that ... anything isn't bad enough to happen to these people. SUSAN DENTZER: Dudley's suit cites the Harris Methodist Health Plan, along with her former physician and employer, Dr. Jack Hardwick. Dudley says Hardwick stopped referring her to her cancer specialist during critical phases of her illness. She says he wrote, at one point, "no more visits" on a letter from one specialist. When the breast cancer spread to Dudley's jaw and she required more chemotherapy, Hardwick once again refused to give her a referral.
SUSAN DENTZER: What did you think he was saying to you? ROSEMARY DUDLEY: "Go home and die, and save me money." And that's what I said. He was playing God, and deciding who should live and who should die, just to put money in his pocket. |
|||||||||||||||||||
|
Avoiding ERISA |
||||||||||||||||||||
|
SPOKESMAN: Call Congresswoman Cubin now, and say you can't afford this bill. SUSAN DENTZER: The bill in question is sponsored by Representative Charlie Norwood and a bipartisan group of lawmakers. Its most controversial provision would remove a key stumbling block in federal law that has deterred many lawsuits against health plans. Known as ERISA-- the Employee Retirement Income Security Act of 1974-- it effectively prevents many people from recovering damages if a health plan's actions resulted in injury. It also bars many lawsuits against health plans in state courts, where juries have been more inclined to favor plaintiffs with big awards. Richard Carter is a plaintiffs' attorney and adjunct professor at Georgetown University's Law School.
SUSAN DENTZER: In crafting the Texas law, the state legislature tried an end-run around ERISA. DOCTOR: How you doing? SUSAN DENTZER: The statute regulates the quality of care, an area of
regulation typically left to states, rather than health insurance benefits,
the area generally governed by ERISA. JERRY PATTERSON, Texas Association of Health Plans: What I'm really concerned with is that the Congress will use the Texas example without knowing what the Texas example proves, for something that they pass in this next session. SUSAN DENTZER: Jerry Patterson heads the Texas Association of Health Plans, which represents more than 20 HMOs and other health insurers. He and other opponents of the law argue that it will eventually trigger a flood of lawsuits and huge damage awards. In turn, they say, that will drive up health insurance costs, and cause thousands of Texans to lose their coverage. But the legislation's supporters, including Texas Insurance Commissioner Jose Montemayor, note that the direst predictions haven't yet come to pass. JOSE MONTEMAYOR: There have not been a deluge of lawsuits, to be very, very sure. It has been a real success story. It largely allowed us to put in place a system of consumer protections that I believe is at the leading edge in the rest of the country. SUSAN DENTZER: Richard Evans is a lobbyist for the Texas Chamber of Commerce. He argues many prospective suits have been put on hold while a federal appeals court reviews the Texas law. RICHARD EVANS: We think the plaintiff's bar is sort of waiting in the wings until we have that first case adjudicated, and then move forward with probably a number of cases they've waited to file. SUSAN DENTZER: But Rosemary Dudley's attorney, George Parker Young, insists that prediction is overblown. GEORGE PARKER YOUNG: It's expensive to bring these cases. You've got to have managed care experts and medical experts, and the HMOs defend these things like the tobacco companies do. I mean, it's no-holds-barred, scorched earth, most expensive lawyers they can find.
|
||||||||||||||||||||
| Working with an independent review | ||||||||||||||||||||
|
DR. ROBERT SLOANE: The patients apparently think it's a success. I've not heard any physician say that he is unhappy with that process. I think the health plans would acknowledge that it's a success, also. SUSAN DENTZER: Dr. Robert Sloane is a Fort Worth trauma surgeon who chairs the Council on Legislation for the Texas Medical Association, the largest physicians group in the state. DOCTOR: Just take the fluid out of the...
DR. ROBERT SLOANE: We've had in the two years about 700 cases that have been requested for review by the patient. Out of those 700, roughly half have sustained the HMOs behavior and decision. SUSAN DENTZER: The other half of the time, the independent reviews have reversed the plans. DR. ROBERT SLOANE: Those patients have felt, I think, that they've had their day in court.
PHILLIP DUNNE: There is a plan that I'm familiar with where 90 percent of the cases that we see from them, we uphold their decision. Contrarily, we see a number of plans where we're reversing up to 80 percent-- I'm being honest-- sometimes maybe 90 percent of the time.
AMY THOMPSON: He was kicked out of the daycare for aggressive behavior. I mean, he had just turned four -- biting, kicking, screaming, kind of acting like 2-year-old behavior. SUSAN DENTZER: Outpatient therapy and medication for attention deficit disorder failed to help. Bryan's physician at Cook Children's Hospital in Fort Worth then diagnosed him with bipolar disorder, a condition he apparently inherited from his father. The doctor recommended that Bryan be hospitalized for intensive observation and treatment. But the company that administered mental health benefits for Thompson's HMO said no. SUSAN DENTZER: What did they say?
SUSAN DENTZER: After rounds of fruitless phone calls to the company, Thompson pressed for independent review. The IRO concluded that her health plan, HMO Blue of Texas, should have paid for more of his recommended care. HMO Blue of Texas says that for various reasons, the case should never have gone to the IRO. Nonetheless, it has agreed to abide by the decision. Bryan, meanwhile, is on other medication, and continues in outpatient therapy. His mother says he's a new child. AMY THOMPSON: He's slowed down a whole lot. Normally, he would not be sitting over there and doing that. I mean he would be bouncing off the walls in here. And, I mean, he's just doing fantastic.
JERRY PATTERSON: We're big fans of the external review, or independent review procedure, very much so. SUSAN DENTZER: In spite of the acceptance independent review, it is currently in legal jeopardy. Last year, a federal judge struck down that section of the Texas law, arguing it was preempted by ERISA. That decision is currently on appeal. Legal experts say unless Congress acts soon to change the law, Texas's novel effort to regulate health plans could be headed for the Supreme Court. |
||||||||||||||||||||
![]()
home | newshour index | search | forum | shields & gigot | letters | essays & dialogues | off camera | pbs online
Copyright © 1999 MacNeil-Lehrer Productions. All Rights Reserved.
 SUSAN
DENTZER: While members of Congress debate a so-called "Patients
Bill of Rights," the eyes of politicians and many health policy
experts are on Texas. That's where a controversial law was passed in
1997. Texas became the first state in the nation to allow patients to
sue managed care plans for damages in state court if they were denied
medically necessary care. So far, four lawsuits have gone to court,
including that of 66-year-old Rosemary Dudley, a former nurse who suffers
from advanced breast cancer.
SUSAN
DENTZER: While members of Congress debate a so-called "Patients
Bill of Rights," the eyes of politicians and many health policy
experts are on Texas. That's where a controversial law was passed in
1997. Texas became the first state in the nation to allow patients to
sue managed care plans for damages in state court if they were denied
medically necessary care. So far, four lawsuits have gone to court,
including that of 66-year-old Rosemary Dudley, a former nurse who suffers
from advanced breast cancer. ROSEMARY
DUDLEY: He said, "You can go home, and we will treat symptoms as
they occur," which means that he would give me pain medicine. And
I just looked at him. I was so angry to think that he was denying me
this chance.
ROSEMARY
DUDLEY: He said, "You can go home, and we will treat symptoms as
they occur," which means that he would give me pain medicine. And
I just looked at him. I was so angry to think that he was denying me
this chance. 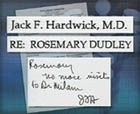 SUSAN
DENTZER: Dudley claims Hardwick's reason was that he would lose income
from the Harris plan if he referred too many of his patients to costly
specialists. Neither officials of the Harris plan nor Dr. Hardwick would
comment on camera about Dudley's lawsuit. However, Hardwick's attorney
said in a statement: "Dr. Hardwick's patients always received care
that met or exceeded standards for our community, and the patients were
seen by specialists when appropriate …We are confident that the
courts will agree." The Texas lawsuits, including Dudley's, are
now in the courts. Meanwhile, states like Georgia and California have
enacted similar bills, and a number of other states are also considering
legislation. Coupled with the drive in Washington for a Patients' Bill
of Rights, these trends have prompted a high-stakes lobbying campaign
by health plans and employers.
SUSAN
DENTZER: Dudley claims Hardwick's reason was that he would lose income
from the Harris plan if he referred too many of his patients to costly
specialists. Neither officials of the Harris plan nor Dr. Hardwick would
comment on camera about Dudley's lawsuit. However, Hardwick's attorney
said in a statement: "Dr. Hardwick's patients always received care
that met or exceeded standards for our community, and the patients were
seen by specialists when appropriate …We are confident that the
courts will agree." The Texas lawsuits, including Dudley's, are
now in the courts. Meanwhile, states like Georgia and California have
enacted similar bills, and a number of other states are also considering
legislation. Coupled with the drive in Washington for a Patients' Bill
of Rights, these trends have prompted a high-stakes lobbying campaign
by health plans and employers. 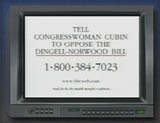 SPOKESMAN
IN COMMERCIAL: I could be sued for providing health insurance for my
employees? That could cost me my business!
SPOKESMAN
IN COMMERCIAL: I could be sued for providing health insurance for my
employees? That could cost me my business!  RICHARD
CARTER: The practical effect of ERISA is that for people in HMOs, or
in any managed care organization, their right to bring a suit for a
denial of benefits or improper utilization review is reduced to almost
nothing. It's been the subject of a number of cases where the judges
have said in the strongest language possible that "this is a crazy
result, but there is nothing we can do under the law." And the
law needs to be changed.
RICHARD
CARTER: The practical effect of ERISA is that for people in HMOs, or
in any managed care organization, their right to bring a suit for a
denial of benefits or improper utilization review is reduced to almost
nothing. It's been the subject of a number of cases where the judges
have said in the strongest language possible that "this is a crazy
result, but there is nothing we can do under the law." And the
law needs to be changed.  In
effect, the legislature said people could sue for damages in Texas courts
if their health plans failed to exercise ordinary care in making treatment
decisions. Now that many in Congress want to make sure other states
can do the same, Texans are debating the results of their own law.
In
effect, the legislature said people could sue for damages in Texas courts
if their health plans failed to exercise ordinary care in making treatment
decisions. Now that many in Congress want to make sure other states
can do the same, Texans are debating the results of their own law.  SUSAN
DENTZER: Has the Texas law produced any of the results that either its
supporters or opponents claimed? Most observers think the verdict isn't
yet in. What is clear is that for a variety of reasons, only a handful
of lawsuits has resulted to date, and most people agree that the one
clear benefit of the law has been a process of independent external
review of health plan decisions that seems to work well for everybody.
SUSAN
DENTZER: Has the Texas law produced any of the results that either its
supporters or opponents claimed? Most observers think the verdict isn't
yet in. What is clear is that for a variety of reasons, only a handful
of lawsuits has resulted to date, and most people agree that the one
clear benefit of the law has been a process of independent external
review of health plan decisions that seems to work well for everybody.
 SUSAN
DENTZER: Sloane says the new review process gives people denied care
the right to an independent review of that decision by qualified professionals.
They have the power to overrule the plan and force it to pay.
SUSAN
DENTZER: Sloane says the new review process gives people denied care
the right to an independent review of that decision by qualified professionals.
They have the power to overrule the plan and force it to pay.  SUSAN
DENTZER: The independent review process begins after a plan has denied
care, or refused to pay for care that has already been delivered. A
patient can first appeal the decision through the plan's own in-house
review process, but if that's unsuccessful, he or she can then turn
to the Independent Review Organization, or IRO. The IRO obtains all
relevant medical records, and sends the case to one of several hundred
qualified health care providers for review. In life-threatening situations,
the review can take as little as one to five days. The cost is borne
by the health plan. Phillip Dunne is chief executive officer of the
Texas Medical Foundation, one of two IROs in the state. He says the
process has shown that some plans seem to be denying care more than
others.
SUSAN
DENTZER: The independent review process begins after a plan has denied
care, or refused to pay for care that has already been delivered. A
patient can first appeal the decision through the plan's own in-house
review process, but if that's unsuccessful, he or she can then turn
to the Independent Review Organization, or IRO. The IRO obtains all
relevant medical records, and sends the case to one of several hundred
qualified health care providers for review. In life-threatening situations,
the review can take as little as one to five days. The cost is borne
by the health plan. Phillip Dunne is chief executive officer of the
Texas Medical Foundation, one of two IROs in the state. He says the
process has shown that some plans seem to be denying care more than
others.  SUSAN
DENTZER: Amy Thompson and her 4-year-old son Bryan are among the beneficiaries
of the independent review process. When Bryan was a toddler, his mother
thought he suffered from an especially bad case of the terrible twos.
Then, almost a year ago, Bryan's behavior grew worse.
SUSAN
DENTZER: Amy Thompson and her 4-year-old son Bryan are among the beneficiaries
of the independent review process. When Bryan was a toddler, his mother
thought he suffered from an especially bad case of the terrible twos.
Then, almost a year ago, Bryan's behavior grew worse.  AMY
THOMPSON: That it wasn't medically necessary at the time, that the diagnosis
... and I told them that I had the book that bipolar was listed as a
serious mental illness that should be listed, and they told me that,
well, he was not five. And I said, "There's no age limit in here."
AMY
THOMPSON: That it wasn't medically necessary at the time, that the diagnosis
... and I told them that I had the book that bipolar was listed as a
serious mental illness that should be listed, and they told me that,
well, he was not five. And I said, "There's no age limit in here."
 SUSAN
DENTZER: Today, it's virtually a universal belief in Texas that independent
review has worked for everybody. The law's proponents say that, together
with the expanded right to sue, the independent review process has made
health plans more careful in evaluating whether care is genuinely needed.
And even the health plans are vocal in their support of independent
review. Health Plan Representative Jerry Patterson.
SUSAN
DENTZER: Today, it's virtually a universal belief in Texas that independent
review has worked for everybody. The law's proponents say that, together
with the expanded right to sue, the independent review process has made
health plans more careful in evaluating whether care is genuinely needed.
And even the health plans are vocal in their support of independent
review. Health Plan Representative Jerry Patterson.