The Children in ‘The Medicated Child’ Have Grown Up, and Mental Health Treatment for Kids Has Evolved
August 30, 2023
Share
When Jessica Kennedy was five years old, she was diagnosed with bipolar disorder. Her mother told FRONTLINE in the 2008 documentary The Medicated Child that she couldn’t go a day without taking medication to stabilize her mood.
“As long as I’m taking medication, then I’ll be fine,” Kennedy told FRONTLINE when she was 12. “It’s the only way to keep me settled down. Taking my medication makes me more calmer, more like I’m supposed to be.”
Now 28, Kennedy has been off of psychiatric medications for a decade. She said while they appeared to fix her behavioral issues because she was more compliant, her performance in school suffered, and her head became clearer once she stopped taking them. Therapy now helps Kennedy deal with what she said her therapist believes are symptoms of autism.
“The meds were dulling literally all of my emotions to the point where it didn’t fix the problem,” she told FRONTLINE in a recent interview. “I still had them, but I wasn’t able to express them.”
The Medicated Child documented the rise of bipolar disorder diagnoses among children in the mid-1990s to late-2000s. That came along with a rise in the prescription of antipsychotic drugs to treat them, despite a dearth of independent research into their safety and efficacy in children at the time. Since then, studies have found that prescriptions of these powerful medications to children have declined, and a smaller number of children are taking them for bipolar disorder. Still, experts remain concerned about the lack of access to care beyond medication amid a worsening youth mental health crisis.
Diagnoses shift and antipsychotics prescriptions decline
By the mid-2000s, a growing number of children were being diagnosed with bipolar disorder, a controversial trend as the disorder was previously thought to only exist in adults.
That rise followed a series of studies at Massachusetts General Hospital led by Dr. Joseph Biederman. In a noteworthy 1996 paper, Biederman’s group theorized that many children who were diagnosed with attention-deficit/hyperactivity disorder (ADHD) also met the criteria for bipolar disorder.
The documentary showed that the rapid rise in bipolar diagnoses was coupled with a rise in prescriptions for antipsychotic medications and mood stabilizers, used to quell disruptive behavior and mood swings in children.

In the years after 2008, when the documentary first premiered, there was growing concern that bipolar was not the appropriate diagnosis for all of the behavioral patterns providers were seeing. Researchers tried to address this in 2013, in the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM) — the guide doctors use to diagnose mental illnesses. They added a new diagnostic category for children exhibiting strong emotional outbursts and frequent irritability called disruptive mood dysregulation disorder.
The new diagnosis appeared in the chapter on depression in the manual, which can mean that antidepressants often become the first line of treatment, said Dr. Eric Youngstrom, a clinical psychologist who co-chairs the Work Group for Child Diagnosis for the International Society for Bipolar Disorders. But Youngstrom also said there are multiple studies and analyses that show that antidepressants aren’t very effective for treating disruptive behavior problems.
“So there’s this group of kids that the book is trying to decide, do we think of it as a behavior problem or do we think of it as a depressive problem?” he said.
The World Health Organization chose the former, opting to add a new sub-diagnosis to an existing behavior disorder, instead of adding disruptive mood dysregulation disorder to its diagnostic manual.
Since The Medicated Child aired, studies have shown a decline in antipsychotics prescribed to children. Two recent studies found that antipsychotic prescriptions declined from the late-2000s to late-2010s in both privately-insured children and kids insured through Medicaid.
Dr. Stephen Crystal and Dr. Greta Bushnell, two of the studies’ authors, said the decline in antipsychotic prescriptions for children was driven by new safety guidelines, as well as stricter requirements for prescribing such drugs to children on Medicaid. Several states require providers to receive approval from the state Medicaid agency before prescribing antipsychotics to children, an extra hurdle correlated with the decrease in prescriptions. Bushnell and Crystal concluded it had spillover effects on privately insured children too.
The researchers also observed a decline in the number of children taking antipsychotics specifically to treat bipolar in both groups — privately-insured and on Medicaid.
“That tendency to attribute the mood issues, mood swings, challenging behavior [to] bipolar has been somewhat debunked,” said Crystal, director of the Center for Health Services Research at Rutgers Institute for Health, Health Care Policy and Aging Research.
But medication can still be an effective treatment for some children. For kids who are dealing with mood dysregulation disorders, including bipolar, providers and families’ decision on whether to medicate “has to take into account the risk of not treating” said Dr. Janet Wozniak, director of the Pediatric Bipolar Disorder Clinical and Research Program at Massachusetts General Hospital, in a hospital presentation in January 2020. Delaying treatment, she said, can worsen outcomes into adulthood.
“It’s terrifying writing these prescriptions; it’s terrifying getting these prescriptions. But what’s more terrifying [is] not treating,” she said. “Because there’s suicide attempts, there’s poor judgement, there’s reckless behaviors, there’s criminal arrest, abuse and addiction.”
Growing need for therapy outpaces resources
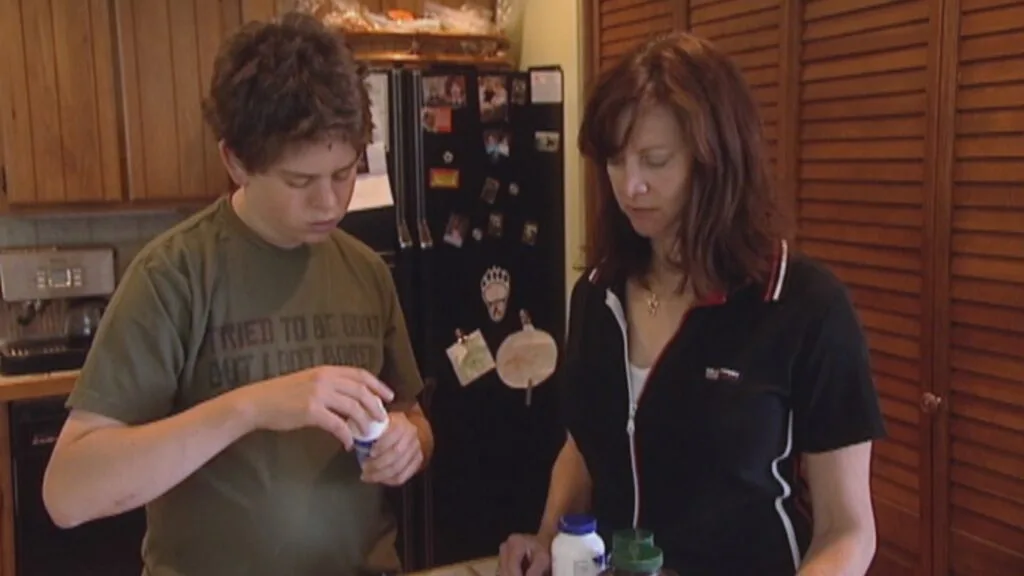
Jacob Solomon was diagnosed with bipolar disorder, ADHD and autism and later Asberger’s syndrome when he was a kid. At one point, he was taking eight different medications at once.
Solomon was 16 when he appeared in The Medicated Child. At 32, he still identifies with each of those disorders, and after years of trial-and-error and consistent care, he said he feels like he’s found what works for him.
“I really think the fact that I am where I am now, after going through all of that, that’s what matters,” he said in a recent interview with FRONTLINE. “I got through it.”

Solomon works for United Airlines as a flight training scheduler and as a DJ in Denver. He produces and records his own music and just finished his first album. He now takes four medications that he said help, but he’s found the most clarity by going to the gym every day. Solomon isn’t in therapy right now — he’s currently using ChatGPT as a stand-in counselor — but said he wants to return to therapy soon.
Clinical guidelines advise that children receive counseling in conjunction with or before turning to psychiatric medication. However, Bushnell and Crystal’s study of privately-insured children from 2007 to 2017 found that only half of the children prescribed antipsychotics had visited a psychiatrist or had received therapy.
Dr. Laura Chavez, a researcher at Nationwide Children’s Hospital in Ohio who has studied antipsychotic use and anxiety medication use in children, observed a similar dynamic in a 2023 study that she co-authored: While anxiety diagnoses increased from 2006 to 2018, office visits for therapy decreased.
And the number of children and adolescents reporting symptoms of anxiety and depression has grown in recent years. ADHD diagnoses are also on the rise.
Chavez said that despite those growing mental health needs, a shortage of resources has contributed to a decline in child and adolescent therapy visits.
“Primary care providers are really facing an onslaught of patients that are really needing help, but have maybe the least resources available to them to deliver mental health,” Chavez told FRONTLINE. “It’s not a problem we’re going to be able to prescribe our way out of.”

Kennedy and Solomon grew up with medication as a main form of treatment, and they both said that they have now found ways to manage their mental health that don’t entirely depend on it. They live on their own — something they said others didn’t think was possible when they were children. Kennedy is planning to make a career of working with children, working toward a degree in early childhood education.
Looking back at her childhood, Kennedy said, “While I didn’t have the vocabulary to articulate a lot of things, which made things a lot more difficult, I feel like paying more attention to the kid, and asking the kid, and therapy would be a huge help.”
Watch the full documentary The Medicated Child:

Email:
julia_ingram@wgbh.orgRelated Documentaries
Latest Documentaries
Related Stories
Related Stories
Explore
Policies
Teacher Center
Funding for FRONTLINE is provided through the support of PBS viewers and by the Corporation for Public Broadcasting, with major support from Ford Foundation. Additional funding is provided the Abrams Foundation, Park Foundation, John D. and Catherine T. MacArthur Foundation, Heising-Simons Foundation, and the FRONTLINE Trust, with major support from Jon and Jo Ann Hagler on behalf of the Jon L. Hagler Foundation, and additional support from Koo and Patricia Yuen. FRONTLINE is a registered trademark of WGBH Educational Foundation. Web Site Copyright ©1995-2025 WGBH Educational Foundation. PBS is a 501(c)(3) not-for-profit organization.