The Vaccine War
April 27, 2010
53m
Inside the raging debate: parents' right to make choices versus the needs of a community
The Vaccine War
April 27, 2010
53m
Share
Public health scientists and clinicians tout vaccines as one of the greatest achievements of modern medicine. But for many ordinary Americans vaccines have become controversial. Young parents are concerned at the sheer number of shots — some 26 inoculations for 14 different diseases by age 6 — and follow alternative vaccination schedules. Other parents go further. In communities like Ashland, Oregon, up to one-third of parents are choosing not to vaccinate their kids at all. This is the vaccine war: On one side sits scientific medicine and the public health establishment; on the other a populist coalition of parents, celebrities, politicians and activists.
Produced by
Transcript
Credits
Journalistic Standards
Support provided by:
Learn More
Most Watched
The FRONTLINE Newsletter
Related Stories

Officials Say Social Media Plays a Role in the Spread of Vaccine Misinformation

California Approves Strict New Vaccine Requirements for Children

What’s Next for the Vaccine Debate? Live Chat 3/25 3:00 pm ET

Seth Mnookin: How the Vaccine War Has Changed

“The Time Was Right to Revisit This Issue”: Behind the Scenes of “The Vaccine War”
A Very Short History of Vaccines in America

What Are the Vaccine Exemption Laws in Your State?

Could Your Pediatrician Spot a Disease Made Rare By Vaccines?

Forum: What Do Doctors Think About America’s “Vaccine War”?
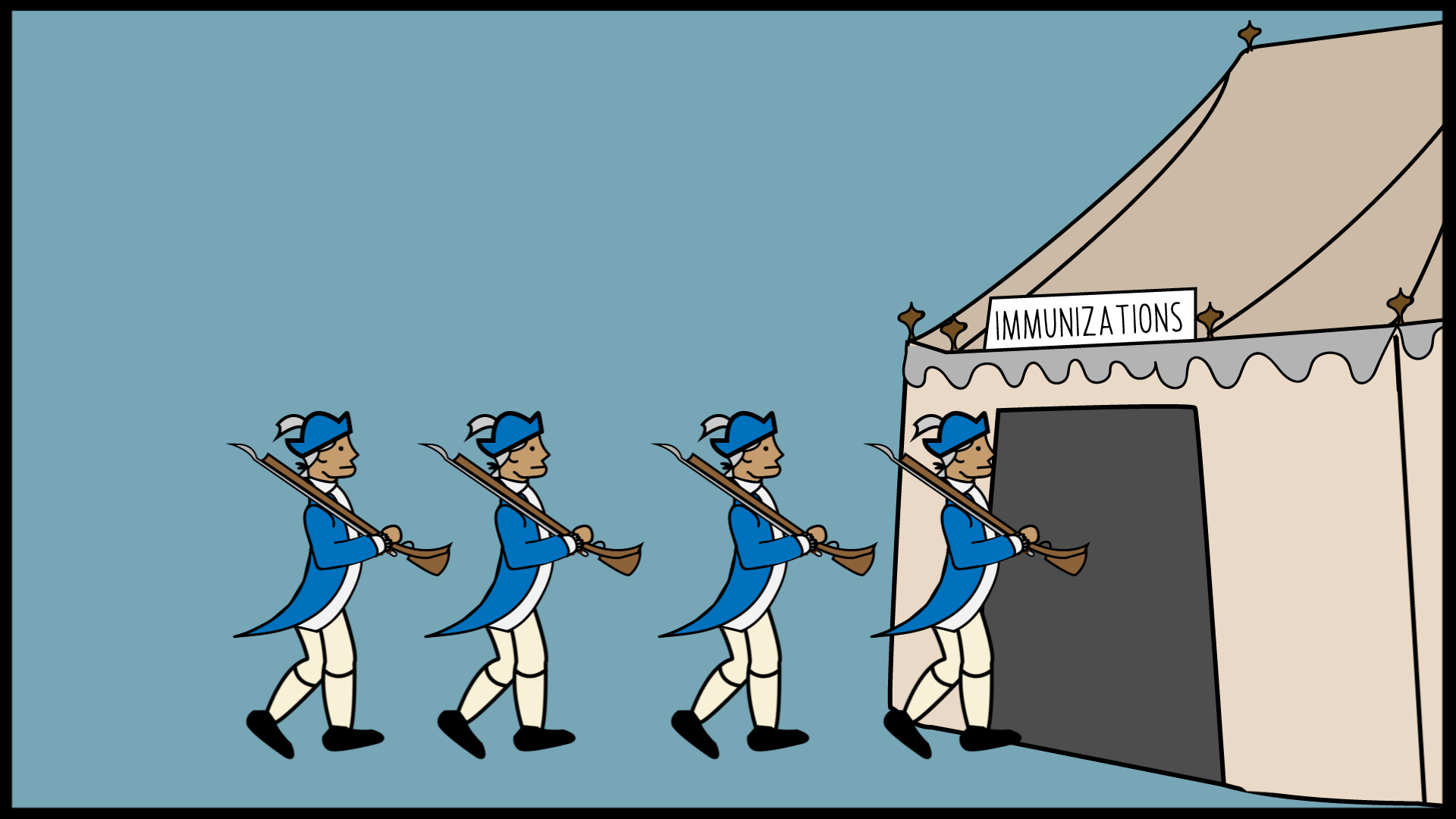
Dr. Anthony Fauci: Risks From Vaccines Are “Almost Nonmeasurable”

Jenny McCarthy: “We’re Not An Anti-Vaccine Movement … We’re Pro-Safe Vaccine”
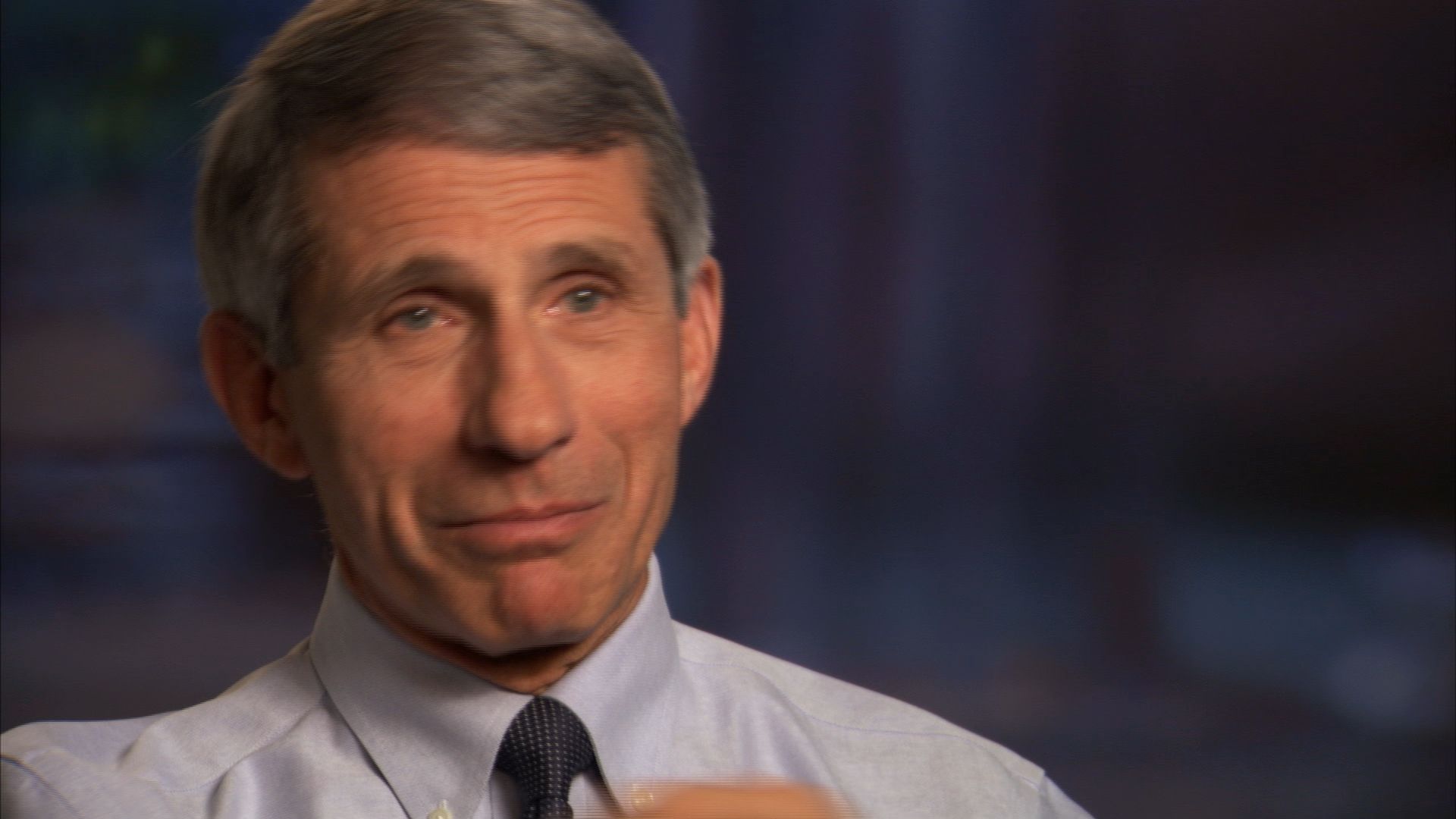
Dr. Paul Offit: “A Choice Not To Get a Vaccine Is Not a Risk-Free Choice”
Dr. Cynthia Cristofani: Not Vaccinating Children is a “Twofold Tragedy”

Dr. Robert W. Sears: Why Partial Vaccinations May Be an Answer

Alvaro and Myriam Fontan: Herd Immunity is the “Only Thing” to Protect a Child Like Ours

J.B. Handley: No Study Shows “Vaccines Didn’t Cause My Son’s Autism”

Coming in March on FRONTLINE

CDC Urges Measles Vaccinations as Number of Cases Exceeds 100

Doctors to Parents: Get Your Child Vaccinated, Or Get Out

Why Aren’t Parents Vaccinating Their Children?

Report: No Link Between Vaccines and Autism
Related Stories

Officials Say Social Media Plays a Role in the Spread of Vaccine Misinformation

California Approves Strict New Vaccine Requirements for Children

What’s Next for the Vaccine Debate? Live Chat 3/25 3:00 pm ET

Seth Mnookin: How the Vaccine War Has Changed

“The Time Was Right to Revisit This Issue”: Behind the Scenes of “The Vaccine War”
A Very Short History of Vaccines in America

What Are the Vaccine Exemption Laws in Your State?

Could Your Pediatrician Spot a Disease Made Rare By Vaccines?

Forum: What Do Doctors Think About America’s “Vaccine War”?
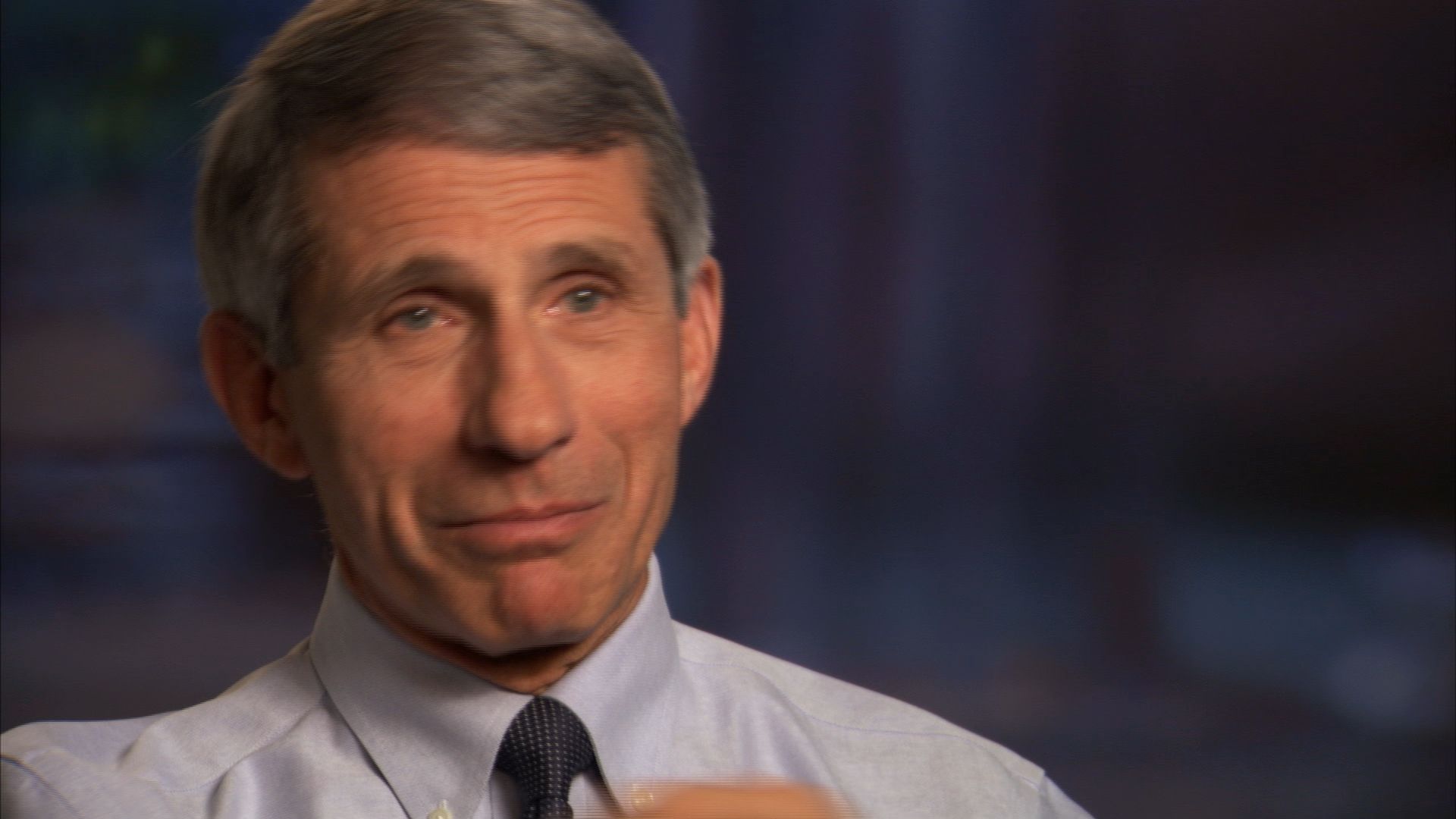
Dr. Anthony Fauci: Risks From Vaccines Are “Almost Nonmeasurable”

Jenny McCarthy: “We’re Not An Anti-Vaccine Movement … We’re Pro-Safe Vaccine”
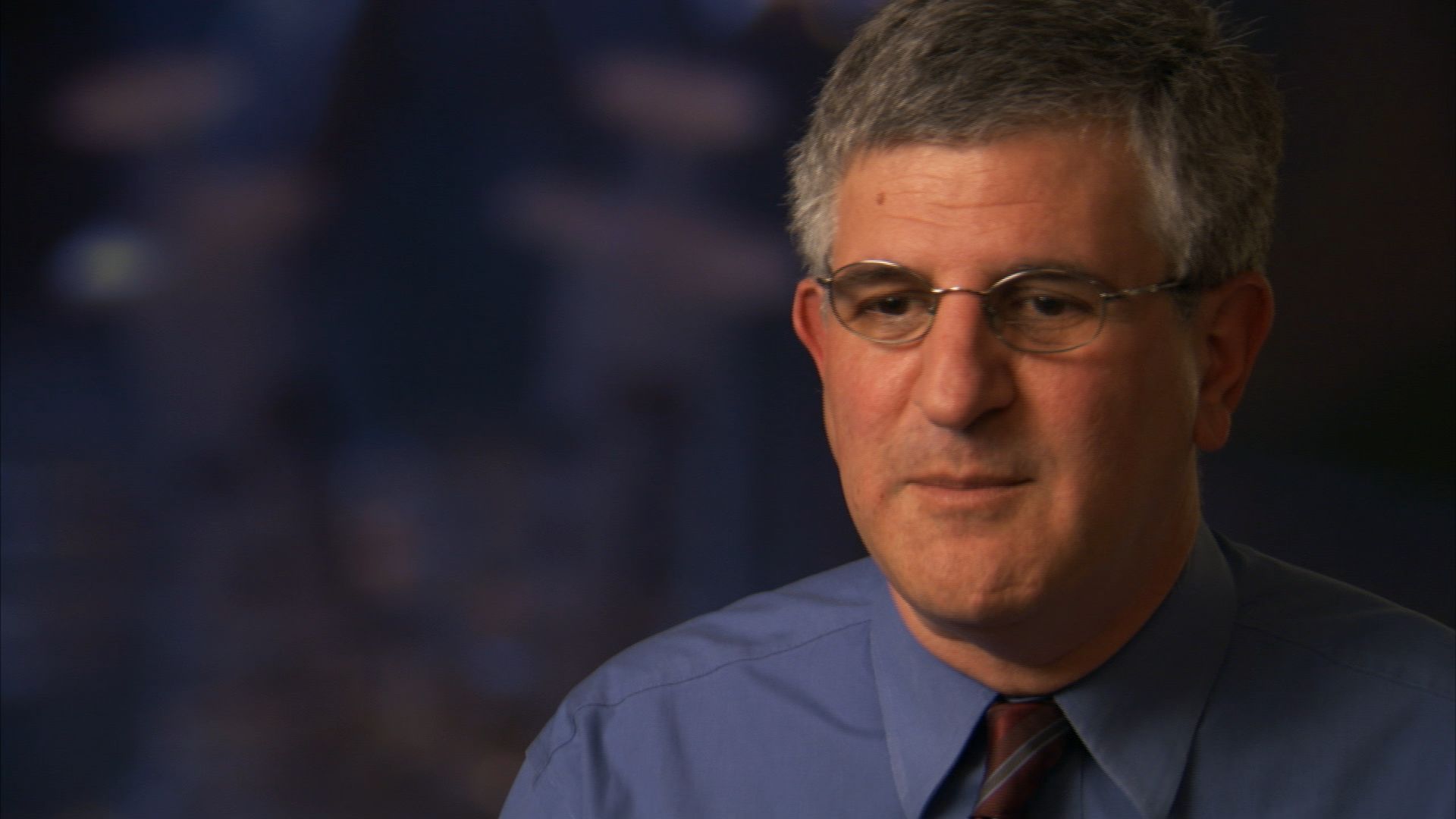
Dr. Paul Offit: “A Choice Not To Get a Vaccine Is Not a Risk-Free Choice”
Dr. Cynthia Cristofani: Not Vaccinating Children is a “Twofold Tragedy”

Dr. Robert W. Sears: Why Partial Vaccinations May Be an Answer

Alvaro and Myriam Fontan: Herd Immunity is the “Only Thing” to Protect a Child Like Ours

J.B. Handley: No Study Shows “Vaccines Didn’t Cause My Son’s Autism”

Coming in March on FRONTLINE

CDC Urges Measles Vaccinations as Number of Cases Exceeds 100

Doctors to Parents: Get Your Child Vaccinated, Or Get Out

Why Aren’t Parents Vaccinating Their Children?

Report: No Link Between Vaccines and Autism
WRITTEN BY
Jon Palfreman
PRODUCED AND DIRECTED BY
Jon Palfreman and Kate McMahon
DELIVERY ROOM STAFF: [home video] What a cute little face. Here we come! It’s a girl! She’s beautiful. What’s her name? Rachel.
NARRATOR: A new life begins. Out of her mother’s womb, Rachel Murphy is now surrounded by a new world filled with countless germs. Modern medicine will do what it can to protect her.
NURSE: It’s just a tiny little stick.
NARRATOR: Barely an hour old, Rachel gets her first shot, against hepatitis B. This is the first of up to 35 inoculations she will get in the next six years of her life to fight 14 diseases.
[on screen: Diphtheria, Hib disease, hepatitis A, hepatitis B, influenza, measles, meningitis, mumps, pertussis, pneumonia, polio, rotavirus, rubella, tetanus]
NARRATOR: Public health doctors celebrate vaccines as one of medicine’s shining achievements.
PAUL OFFIT, M.D., Children’s Hospital of Philadelphia: They’ve increased our lifespan by 30 years. Hib would cause 20,000 to 25,000 cases a year. Gone. I mean, polio would paralyze, you know, tens of thousands of children every year. Gone. I mean, diphtheria was the most common killer of teenagers in the 1920s. Gone. I mean, you know, vaccines— the benefit of vaccines is clear.
MELINDA WHARTON, M.D., M.P.H., Centers for Disease Control and Prevention: Well, there’s now 16 diseases that are preventable by vaccination for children. Fourteen of those are diseases that we vaccinate infants and young children for, and two of them are diseases that we vaccinate adolescents. From my point of view, being able to prevent 16 diseases by vaccination is a really good thing.
NARRATOR: But this public health miracle has been losing ground. Since we first reported on the vaccine war in 2010, more parents across America have decided not to fully vaccinate their children. Like all wars, this one has casualties.
NEWSCASTER: Health officials suspect someone who was out at Disneyland resort in mid-December had the measles, and that’s how the disease spread.
NEWSCASTER: The measles outbreak that began at Disneyland in December has now spread to more than 90 people in the U.S.
NARRATOR: December 2014, the U.S. experienced a major measles outbreak, a disease that had been eliminated from this country 15 years ago.
NEWSCASTER: This has got to be so frustrating for public health officials.
SETH MNOOKIN, Assoc. Dir., Science Writing, MIT: Now it’s spread to over 100 infections to different states around the country. Because of that, it’s something that’s gotten a lot of attention.
NARRATOR: Seth Mnookin is a science writer at MIT who has reported extensively on the vaccine debate.
SETH MNOOKIN: A single person infected with this disease can have implications that are going to go on for months. Because it is the most infectious microbe known to humankind, the efforts to contain it, the efforts to track down everyone that the infected person has come in contact with are just incredibly, incredibly expensive.
NARRATOR: The CDC tracks outbreaks of infectious diseases around the country from its center in Atlanta. Over the last 15 years, they’ve detected pockets of diseases like whooping cough and measles. The CDC uses forensic techniques to dissect in fine detail how dangerous pathogens can spread.
They analyzed one such event, a measles outbreak that struck an under-vaccinated area of San Diego in 2008. Like most measles outbreaks, it came from abroad. It began when an infected 7-year-old returned from a family vacation in Switzerland on January 15th.
The child gave measles to two siblings, and collectively, they infected classmates at the San Diego Cooperative Charter School in Linda Vista. A visit to the Children’s Clinic of La Jolla spread the infection to four others. One of these, an infant, flew on a plane to Hawaii, where she was intercepted and quarantined. The other 250 passengers had to be contacted and tracked.
Dr. Wilma Wooten is San Diego County’s public health officer.
WILMA WOOTEN, M.D., M.P.H., Public Health Officer, San Diego: This entire process resulted in exposures of almost 1,000 individuals, 90 with no proof of immunization, 73 were quarantined, 12 additional actual cases of measles in San Diego.
NARRATOR: Public health officials determined that what allowed measles to enter the community was that kids were not being immunized because their parents were getting around public school immunization rules by using “personal belief exemptions” allowed in states like California.
School principals have found themselves caught on the front lines.
WENDY RANCK-BUHR, Principal, SD Cooperative Charter School: The fact is that some families choose not to immunize their children. And then there are families who have children who are particularly medically sensitive, and they’re in jeopardy because they could get sick from unimmunized children. So it’s a very emotional issue on both sides.
NARRATOR: Across America, the CDC has discovered certain communities with a large population of parents who either do not vaccinate their children or pick and choose which vaccines to permit and how they are scheduled. One such place is Ashland, Oregon.
JENNIFER MARGULIS, Parent, Ashland, OR: This is our neighborhood, and we love it because we can walk everywhere. Ashland is a very safe town compared to almost every place else in America.
NARRATOR: It’s a college town, the home of an annual Shakespeare festival, where a well-off, educated population has easy access to alternative medicines, an organic food co-op and yoga centers. Jennifer Margulis, a writer with a Ph.D. in English, is the mother of four children.
JENNIFER MARGULIS: When my daughter was born in 1999, the nurse bustled in with her tray and said, “OK, it’s time for your hepatitis B vaccine.” And I looked at my daughter and I looked at the nurse and I said, “Isn’t hepatitis B a sexually transmitted disease?” And I said, “Why am I supposed to vaccine my newborn baby against a sexually transmitted disease?” And the nurse got really mad.
NARRATOR: Margulis went on to research and write about vaccines, and in 2009 published a long article about the vaccine debate in Mothering magazine, a magazine promoting a natural lifestyle.
JENNIFER MARGULIS: Why are we giving children so many vaccines? They get four times the number of vaccines than I got when I was child growing up in the ‘70s. As a parent, I would rather see my child get a natural illness and contract that the way that illnesses have been contracted for at least 200,000 years that homo sapiens has been around. I’m not afraid of my children getting chicken pox. There are reasons that children get sick. Getting sick is not a bad thing.
NARRATOR: In common with many other Ashland parents back in 2010, Margulis had decided not to fully vaccinate her other children according to the officially recommended vaccine schedule.
Ashland still has one of the lowest vaccination rates in the country. Because of exemptions, some 28 percent of Ashland’s kids are allowed to attend public school lacking some or all of their required vaccinations.
DONNA BRADSHAW-WALTERS, M.D., Pediatrician, Ashland, OR: So we’re going to need today the D-TAP number 5, your final polio, your second—
NARRATOR: Pediatrician Dr. Donna Bradshaw-Walters worries that these parents may unwittingly bring back diseases that haven’t been seen for decades.
Dr. DONNA BRADSHAW-WALTERS: The possibility of an outbreak is real here in Ashland. We are not living in a bubble, especially in this day and age of international travel. Our Shakespeare festival draws people from all over the world, and it’s just a matter of time before someone comes to here from another area who is unimmunized and who has the disease and brings that disease into our community.
NARRATOR: In fact, Ashland experienced an outbreak of chicken pox in 2014. And given the low rate of vaccination here, the community is at constant risk of other highly infectious and potentially serious diseases like measles or whooping cough taking hold.
There are many pro-vaccine parents in Ashland, like Lorie Anderson, whose son, Evan, is fully vaccinated.
LORIE ANDERSON: It’s an outbreak waiting to happen. And so I don’t just care about my own child. My child may be well protected because of his vaccination. But I hate to see people get hurt, injured, die, have to be quarantined, isolated because of an outbreak that is preventable with a vaccine.
All they have to do is sign an exemption and their kid is exempt from immunization before they go to school. I will try not to be angry. I hope it doesn’t get contentious. It will, though. It will get contentious if there’s an outbreak. If vaccinated children start to get breakthrough disease because of the high rate of unvaccinated children, it probably will get ugly.
NARRATOR: A vast public health infrastructure is committed to preventing such outbreaks—the National Institutes of Health, the Food and Drug Administration, the Centers for Disease Control and Prevention, large vaccine manufacturers. The mainstream medical establishment speaks with one voice—vaccines are a public health miracle far too valuable to put at risk.
Emilio Emini has spent his life making vaccines in America’s pharmaceutical companies. He heads Pfizer’s vaccine operation.
EMILIO EMINI, Ph.D., Pfizer, Inc.: People haven’t seen these diseases in a while, so people become complacent. They don’t vaccinate. And what they wind up doing is putting their children and themselves in considerable risk of a severe disease and infection.
Polio, even though people aren’t worried about it because they haven’t seen much of it, is still present in many parts of the world, and it can easily be introduced into a non-vaccinated population. And from what we’ve seen in other parts of the world, once it’s introduced, it will spread very rapidly and cause a lot of disease.
LUCILLE BALL: [public service commercial] The fear, my friends, is polio. But soon, perhaps within a year, there may be a vaccine.
DESI ARNAZ: Thanks for visiting with us. Hey, kids, how about saying good-bye, huh? Come on! Say bye-bye.
KIDS: Good-bye!
ANTHONY FAUCI, M.D., Dir., Natl. Inst. of Allergy and Infectious Disease: When I was a child and the big scare was polio, where you would see your friends playing ball outside with you, baseball and basketball, and all of a sudden get sick and be in bed, be in an iron lung, and then come out with a deformity, a serious limp or a serious physical disability— that is absolutely frozen in your mind as a very scary scenario.
PAUL OFFIT, M.D., Children’s Hospital of Philadelphia: I think we’re compelled by our own fears. And certainly, for my parents, who— you know, who grew up in the 1920s and ‘30s and ‘40s, saw these infections. They saw what they could do. For them, vaccines was an easy sell.
NARRATOR: Paul Offit is a pediatrician and co-inventor of a vaccine against rotavirus, a pathogen that causes serious fever, vomiting and diarrhea.
Dr. PAUL OFFIT: I grew up in the 1950s and ‘60s. I saw measles. I had measles. I had mumps. I had German measles. I mean, I knew what those diseases could do. I watched my friends also be sickened by those diseases. And so for me, vaccines was an easy sell. I think for people now, young mothers today not only don’t see these diseases, they didn’t even grow up with these diseases. So for them, vaccination becomes a matter of faith.
NARRATOR: But the faith of some parents has eroded. Offit, for example, is seen in some quarters not as a hero for inventing a successful vaccine but as a self-interested entrepreneur whom skeptics have called “Dr. Profit.”
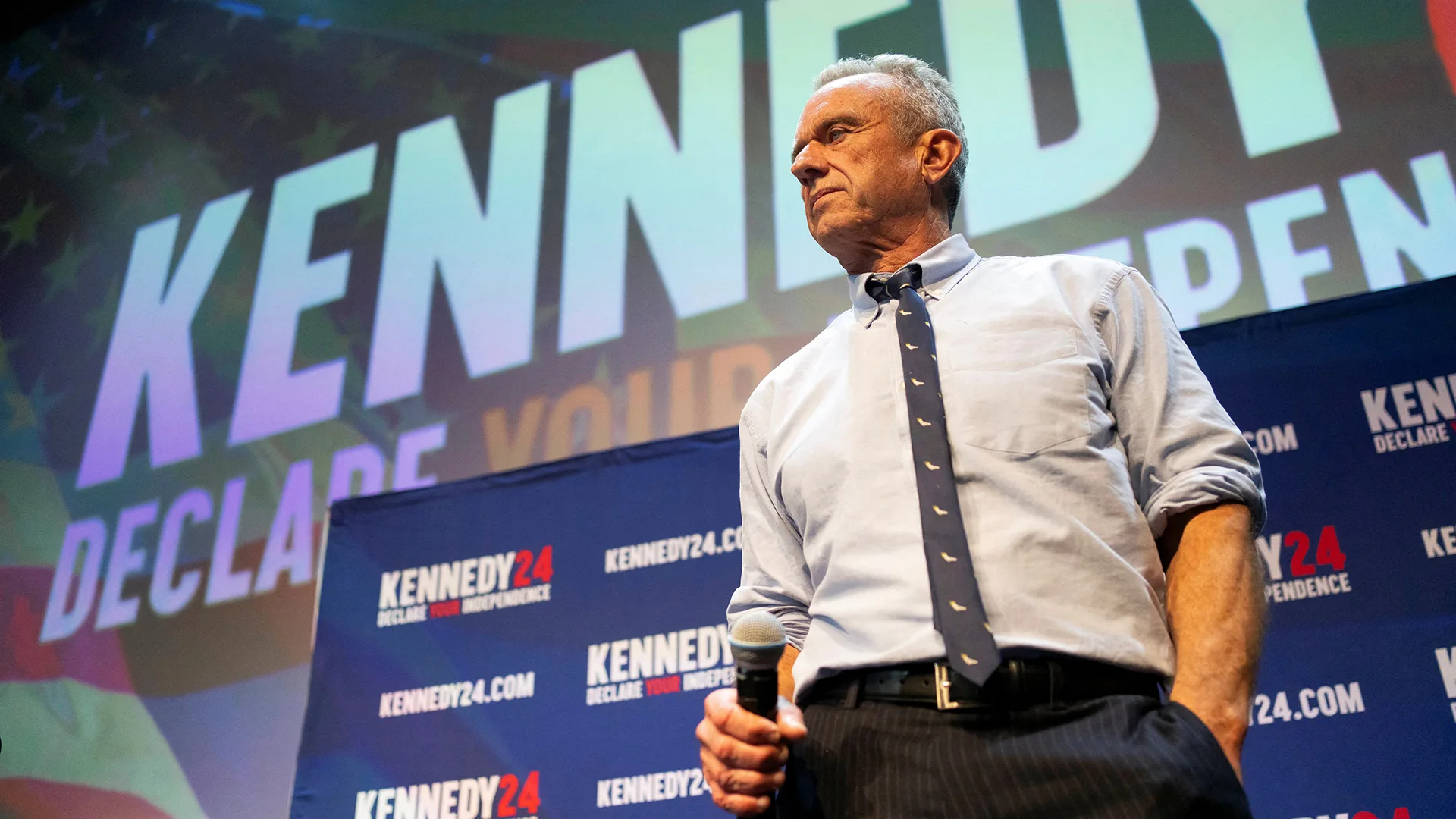
ROBERT F. KENNEDY, Jr.: They all have this guy, Paul Offit. You guys know him? [boos] And he is the poster child for the term “biostitute.” Does not disclose the millions of dollars—
NARRATOR: For such critics, the fact that vaccines have made Offit rich is enough to discount what he is saying. But Offit, a prolific author, makes no apologies.
Dr. PAUL OFFIT: I’m the co-inventor of a rotavirus vaccine, a vaccine that I made in collaboration with Merck. And it’s a vaccine which has caused a dramatic decrease in this country in hospitalization, and has caused already a dramatic decrease in hospitalization and death in some countries in the developing world. I’m enormously proud of that. I would argue that I have an expertise in rotaviruses and-
INTERVIEWER: But you also financially benefit from that vaccine.
Dr. PAUL OFFIT: It’s— it’s— I know this isn’t going to— going to sell. But it doesn’t matter. It doesn’t matter whether I financially have benefited or not. The only thing that mattered is— is— did the vaccine that we created at Children’s Hospital of Philadelphia do what it was claimed to do? Has it prevented hospitalization and suffering and death? And the answer to that question is yes.
JENNIFER MARGULIS: It’s a mistake that we have a vaccine against rotavirus, the vaccine that Paul Offit helped to develop. In the third world, maybe people are dying of rotavirus, but in this country, you have to do back flips to show a death toll of people from rotavirus.
ARTHUR CAPLAN, Ph.D., Center for Bioethics, Univ. of Pennsylvania, 1994-2012: Well, one of the bitter ironies of vaccination is it carries with it the problems of its own success.
NARRATOR: Author and bioethicist Arthur Caplan is an expert on the ethical issues surrounding vaccines.
ARTHUR CAPLAN: Many parents are not thinking about the risk side of disease because they don’t see those diseases. They’ve never seen any child rendered deaf by the mumps. They’ve never seen somebody who’s had a case of polio. I had polio. I was in the hospital, paralyzed legs and neck, for about a year. So I know firsthand what the polio epidemic looked like. I was sort of at the last outbreak before the vaccines really came on line and eliminated it.
NARRATOR: Vaccine-preventable diseases like polio have become rare in the United States, so rare, in fact, that most younger doctors have never seen a case. This is one of the few places where you can see what vaccine-preventable diseases look like. This is a case of pertussis, also known as whooping cough. The audience is made up of paramedic students.
CYNTHIA CRISTOFANI, M.D., Pediatric Intensivist: She can’t breathe, and that’s horrifying for any patient at any age to discover that your airway has closed and you can’t inhale.
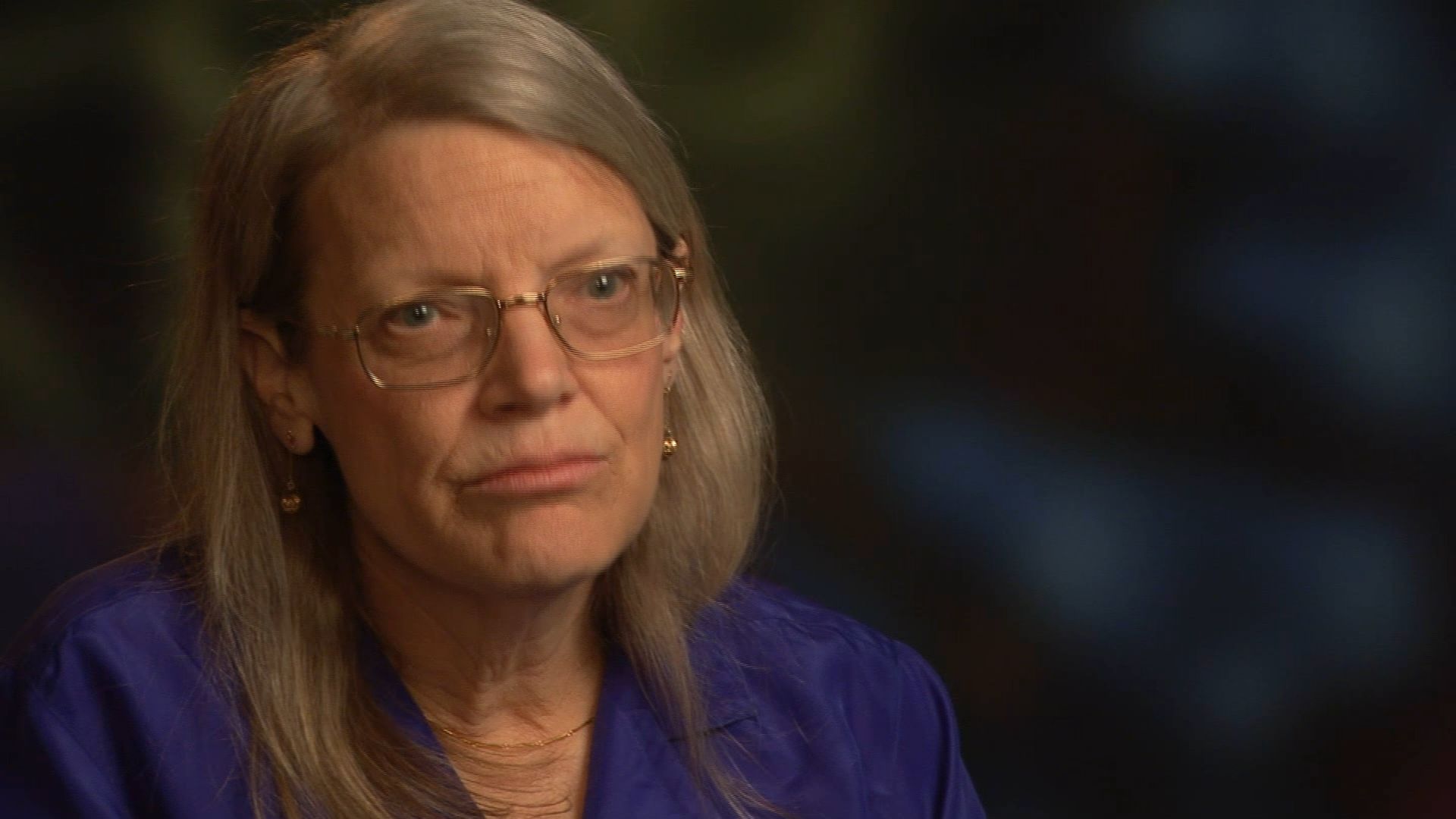
NARRATOR: The teacher, Dr. Cynthia Cristofani, is a pediatric intensivist who treats children in need of critical care. She decided early in her career to document the rare cases of vaccine-preventable illness that turned up in her Portland, Oregon, ICU. She has used the footage to teach other medics how to recognize these diseases.
Dr. CYNTHIA CRISTOFANI: I’m old enough to have seen most of the serious life-threatening illnesses that are largely suppressed and some almost eradicated by the modern vaccines.
This baby was a victim of rotavirus. There’s major fluid deficiency in this child’s tissues. Actually kills over half a million humans annually, most of them elsewhere on the planet.
The community recollection for these diseases has largely disappeared, and so the parents of younger kids who are of vaccine age are unlikely to have had any personal experience. And unless the grandparents or others can tell them what it was like and happen to have had knowledge of somebody who had a severe complication, it’s easy to imagine that these diseases are eradicated.
Those spots are actually something probably none of you have ever seen. They’re chicken pox. This patient had one of the commoner potentially lethal complications of chicken pox. He got strep sepsis from an infected lesion. This child came as close to dying of chicken pox as you can come without doing it. And so I encourage you remember that chicken pox also can cause fatalities. Even though most people used to think of it as a rite of passage in childhood and we all got it, you can do better than that. There’s a vaccine.
This one’s a scary one. This is haemophilus influenza type B meningitis. And he was actually the last patient I ever saw with this disease. I can tell you it was the scourge of pediatrics when I was in training because there was no vaccine. But beware. It could come back if people stop vaccinating.
NARRATOR: But critics have argued that while some vaccines may be life-saving, the current vaccine schedule delivers just too many vaccines too quickly.
JENNIFER MARGULIS: Why are we giving children so many vaccines? There’s no more polio in the United States and there’s no more diphtheria in the United States. And no one, no child, has contracted wild polio since 1979 in the United States. So when do we take polio off the vaccine schedule? When do we say, “Fantastic. The vaccine worked. We figured it out. We don’t have a polio epidemic anymore. Let’s stop vaccinating against polio.”
ANTHONY FAUCI, M.D., Dir., Natl. Inst. of Allergy and Infectious Disease: The number of antigens in the 14 vaccines, including their boosters, which brings it up to somewhere in the 20s— it’s literally a drop in the bucket to the antigens that an infant and a child get exposed to naturally, even if they never got vaccinated with anything.
NARRATOR: Officials like Anthony Fauci have struggled with how to convince parents that the benefits of vaccines far outweigh the risks.
Dr. ANTHONY FAUCI: To say that there is no risk in any vaccine would not be truthful. What is the risk of injecting something into someone’s arm? The risk is that a certain proportion of people will get swelling and a little bit of pain, lasting from an hour to a day. That is a very acceptable risk.
A very, very, very small percentage of people will get an allergic reaction. Namely, there’s a component to the vaccine that they didn’t realize that they were allergic to.
And then there’s a subset of a very, very, very, very small percentage of those who actually could get a serious reaction. But if you look at that, the risk of that is so minisculey small as to be completely outweighed by the benefit.
NARRATOR: The CDC’s Web site tries to convey all these risks accurately, even when scientists are not sure the vaccines are, in fact, responsible. Here’s what it says about the measles vaccine.
WEB SITE: “Severe problems very rare. Several other severe problems have been known to occur after a child gets MMR vaccine. But this happens so rarely, experts cannot be sure whether they are caused by the vaccine or not. These include deafness, long-term seizures, coma, or lowered consciousness, permanent brain damage.”
Dr. PAUL OFFIT: When the CDC communicates risks, they fall into two groups. One is, are those risks that are very rare but, in fact, are real.
DONNA BRADSHAW-WALTERS, M.D., Pediatrician, Ashland, OR: Sometimes very rarely can cause a rash later on—
Dr. PAUL OFFIT: And the other are those risks that have been reported following a vaccine, but for which we have no evidence that the vaccine actually caused the problem. Those, I would argue, are at best theoretical.
BARBARA LOE FISHER, Pres., National Vaccine Info. Ctr.: My son was a bright, precocious, healthy 2-and-a-half-year-old child in 1980 when I took him in for his fourth DPT shot.
NARRATOR: Barbara Loe Fisher runs an independent watchdog organization dedicated to vaccine safety issues. It’s an organization she helped found in 1982 after her son suffered a serious vaccine side effect.
BARBARA LOE FISHER: To make a long story short, after that, he regressed physically, mentally and emotionally and became a totally different child. He was eventually diagnosed with multiple learning disabilities and attention deficit disorder and had to remain in a classroom for the learning disabled throughout his public school.
NARRATOR: Fisher’s organization lobbied successfully for laws that promote vaccine safety. Today, a much safer vaccine has replaced DPT. The laws also created a special vaccine court to evaluate and compensate victims of adverse vaccine side effects.
BARBARA LOE FISHER: Vaccines are pharmaceutical products that inherently carry a risk of injury or death. And that risk can be greater for some than others, particularly for genetic or biological high-risk reasons that have— some of which have been identified and some which have not been identified.
PROTESTERS: [Green our Vaccines rally] Shame on you! Shame on you!
NARRATOR: One fear had come to dominate the vaccine war, the fear that vaccines were responsible for autism, a mysterious disorder that appears to be on the rise. The theory that vaccines could cause autism became well known partly due to the advocacy of celebrities like Jenny McCarthy.
JENNY MCCARTHY, Spokesperson, Generation Rescue: [June 4, 2008] Today I am not a celebrity. Today I am a mom of a child who had autism, who has—
NARRATOR: McCarthy knew little about autism until her son, Evan, received a series of vaccines, including the shot for mumps measles and rubella, the MMR triple shot. A few weeks later, Evan developed seizures and was diagnosed with autism.
JENNY MCCARTHY: So I left that office devastated, hopeless. The next day, or maybe it was even that night, went on Google and typed in “autism.”
NARRATOR: She found the site for Generation Rescue.
JENNY MCCARTHY: So I clicked on Generation Rescue, and I found this community of parents.
NARRATOR: Generation Rescue is run by businessman J.B. Handley. Handley’s son was diagnosed with autism following a series of shots in 2004. At the time, he’d also gone on the Web and discovered a community of parents with stories to share.
J.B. HANDLEY, Founder, Generation Rescue: There were literally tens of thousands of parental reports of children regressing and changing after vaccine appointments.
WEB SITE POSTINGS: “My child was fine before the vaccine.” “The vaccine made Sam autistic.” “He completely changed.” “After the MMR, he wouldn’t look at us.” “Cole just stopped speaking.” “He got the shot, and we started losing him.”
NARRATOR: The vaccine most often blamed in these stories was the MMR triple shot for measles, mumps and rubella.
DONNA BRADSHAW-WALTERS, M.D., Pediatrician, Ashland, OR: Then she would get her second MMR—
J.B. HANDLEY: Few people without kids today realize that when a child goes in for a doctor’s appointment— and they’re required to go in at 2 months, 4 months, 6 months and 12 months to get their initial vaccines— there are literally somewhere between five and seven vaccines lined up on the table that are all given simultaneously within about 12 minutes.
PHYSICIAN: Your daughter will be protected against five things— diphtheria, tetanus, whooping cough, polio and Hib.
J.B. HANDLEY: Well, tens of thousands of parents have reported that their kid was never the same after those appointments. The second data point is the knowledge that vaccines cause brain injury in a small segment of the population. We know that. The federal government knows it. They pay money to kids who’ve been injured that way. This is something that’s been known for years.
And then we also know that the number of vaccines given has risen dramatically. So it does not take a rocket scientist to draw a possible correlation between the vaccines being given and the brain injury that our children are suffering, because autism is brain injury.
NARRATOR: Combining his resources and her celebrity, Handley and McCarthy have been highly effective at organizing a movement of concerned parents.
JENNY McCARTHY: Hi. I’m Jenny McCarthy. I am here today to beg you guys—
NARRATOR: The science that gave the movement its original impetus was a 1998 article by British gastroenterologist Andrew Wakefield in the medical journal The Lancet. He reported on 12 children with gastrointestinal problems, eight of whom developed symptoms of autism following an MMR shot. Wakefield’s theory was that the measles vaccine inflamed the intestines, causing harmful proteins to leak into the bloodstream, eventually damaging the brain and causing autism.
Dr. ANDREW WAKEFIELD: Measles, mumps and rubella given together may be too much for the immune system of some children to handle. Clearly, for the vast majority, it is protective, and we must emphasize that it is just a small cohort of children, we don’t know how large, but who have appeared to have developed the syndrome.
NARRATOR: News of Wakefield’s provocative Lancet article spread across the world, creating fear that measles shots might cause autism.
ERIC FOMBONNE, M.D., McGill University, 2001-2012: There was a dramatic decline in the coverage of young children with measles vaccines.
NARRATOR: Autism expert Eric Fombonne was working in London at the time.
Dr. ERIC FOMBONNE: There were areas, like in urban areas, where it was even lower than 80 percent. And in Ireland in particular, vaccine coverage fell to close to 70 percent, and there was a big outbreak of measles occurring as a result of that fear. One hundred and ten infants were admitted in hospitals in critical conditions, and I think three of them died from measles. And measles is a preventable disease.
Dr. PAUL OFFIT: Parents reasonably thought, “My child was fine. They got an MMR vaccine. Then they developed the first symptoms of autism. Could it have been the MMR vaccine that caused that autism?” That’s a perfectly reasonable question.
NARRATOR: The fact that two events happen close together might mean that they are causally related, but it could also be simple coincidence.
Dr. ERIC FOMBONNE: This vaccination is given at an age where often the first symptoms of autism emerge. And typically, it occurs around 15 or 18 month of age, when these children start to walk, and also when we expect them to develop language, which they usually fail to do.
ANTHONY FAUCI, M.D., Dir., Natl. Inst. of Allergy and Infectious Disease: There are a certain set of diseases that become apparent when children reach a certain age. That’s not cause and effect.
Dr. PAUL OFFIT: Just because one event followed another, it doesn’t mean it was caused by the other. Every morning, the rooster crows, the sun comes up. It doesn’t mean the rooster’s causing the sun to come up. The question is, was it caused by it?
LARRY KING, “Larry King Live”: Isn’t the problem here, Jenny, that people, sometimes casual or listen with one ear, are going to panic and not vaccine at all?
JENNY McCARTHY: Probably. But guess what? It’s not my fault. The reason why they’re not vaccinating is because the vaccines are not safe.
[June 4, 2008] What we are saying is that the number of vaccines given, and the ingredients, like the fricking mercury, the ether, the aluminum, the—
NARRATOR: Vaccine critics questioned not only MMR but the many ingredients in vaccines. These historically have included aluminum, formaldehyde, formalin, yeast protein and a mercury-based preservative called thimerosal used in multi-dose vaccines. One very influential critic is environmental lawyer Robert Kennedy, Jr.
ROBERT F. KENNEDY, Jr.: [June 8, 2004] So the government scientists are acknowledging that even tiny, infinitesimal amounts of mercury, of parts per billion, will cause profound neurological injury in children. The biggest exposure is coming from our own vaccines. When I was a little boy, we only got three vaccines. But my children, five of my six children, got 22 vaccines, beginning in 1989. That’s the thimerosal generation. That’s the vaccine generation.
Dr. ERIC FOMBONNE: So the mercury hypothesis had more plausibility than that for MMR because of the nature of mercury, which is known to be a neurotoxicant. But mercury poisoning does not resemble autism at all. The fact that mercury is a toxicant is not sufficient to claim that the mercury contained in vaccines can lead to autism. So it was critical therefore to follow this hypothesis with properly conducted epidemiological studies.
NARRATOR: Under public pressure, public health agencies decided to act on the side of caution, rather than wait for the results of such epidemiological studies. In 1999, the FDA asked manufacturers to reduce or eliminate thimerosal in vaccines as soon as possible.
Dr. PAUL OFFIT: Unfortunately, I think it precipitated the notion that the thimerosal was doing harm. And from a parent’s standpoint, that again was very understandable. Why would you take something out of vaccines in such a precipitous and frightening manner unless there was a problem?
JENNY MCCARTHY: When I began my crusade for autism, one of the first speeches I gave was, “Is it mercury? Is it the schedule? Is there just too many?” My answer to people, and what I’ve been telling them, is it’s all of the above. We don’t know for sure, which is why we keep saying, “Study it.” But they won’t!
NARRATOR: In fact, around the world, scientists have been studying groups of children, searching for a possible link between vaccines and autism, using the same epidemiological methods that linked smoking to lung cancer.
One country renowned for its epidemiology is Denmark. Unlike the U.S., Danish authorities collect demographic and health data routinely on the entire population in a series of national registers. They know when every child was born, when every child was vaccinated, and when every case of autism was diagnosed.
ANDERS HVIID, Dr. Med. Sci., Statens Serum Institut: It’s sort of a paradise for epidemiologists because we don’t have to work to collect this data. It is available to us.
NARRATOR: Anders Hviid and colleagues at the Statens Serum Institut analyzed data on all the Danish children born between 1991 and 1998, over half a million. They compared two groups, those who had received the MMR triple shot and those who hadn’t. Then they counted the cases of autism in each group and calculated the autism rate.
They found no difference. Children who didn’t get the shot had the same risk of developing autism as those who did. The team published the findings in The New England Journal of Medicine.
Other studies carried out by researchers in Sweden, Britain, Finland and the U.S. also found no association between MMR and autism. Additional evidence came from Japan. The Japanese changed their vaccine schedule in 1993, replacing the MMR triple shot with three separate vaccinations. But following the change, autism rates did not fall. In fact, they appeared to rise, thus making the triple shot an unlikely cause of autism.
The Danish team now went on to investigate the second theory, the mercury preservative thimerosal. It turned out that in Denmark, there was a simple way to test this, as well.
ANDERS HVIID: In Denmark, since the ‘70s, only one vaccine has contained thimerosal, and that was a pertussis vaccine. It contained thimerosal until May, June ‘92. Then the same vaccine continued but without thimerosal.
NARRATOR: Hviid and colleagues found that children who were given pertussis vaccines with thimerosal before 1992 had identical autism rates as children who received mercury-free vaccines after that date.
ANDERS HVIID: We did not find any association between being vaccinated with the thimerosal-containing vaccine and the risk of autism.
NARRATOR: Other studies in the U.S., the U.K. and Canada also found no association between autism and thimerosal. In 2004, the Institute of Medicine carried out its own analysis of the research and concluded, “The body of epidemiological evidence favors rejection of a causal relationship between the MMR vaccine and autism and also between thimerosal-containing vaccines and autism.”
Dr. ANDREW WAKEFIELD: The allegations against me are both unfounded and unjust!
NARRATOR: Then something extraordinary happened. On February 2, 2010, The Lancet retracted Wakefield’s landmark 1998 paper, saying it was scientifically flawed. The Lancet reported that Wakefield’s findings could not be replicated, and it turned out that some of the kids in his small sample had been referred to his study by a lawyer who was suing pharmaceutical manufacturers on the children’s behalf.
A few months later, Wakefield was stripped of his medical license. But despite these revelations, organizations like Generation Rescue came out in strong support of Wakefield, continuing to believe in his science.
Soon after, parents of autistic children who brought class-action lawsuits based on the MMR and thimerosal theories had their hopes dashed by the federal vaccine court.
NEWSCASTER: And good evening to you. We begin tonight with a ruling that affects millions of parents with children who have autism. Families who went to a federal court over these vaccines were told that their case was without scientific or legal merit.
NARRATOR: The vaccine court that Barbara Loe Fisher’s organization had helped set up issued a strongly worded ruling on March 12, 2010, denying a link between autism and vaccines.
ANDERS HVIID: Scientifically, I think the matter is settled. But I don’t think that— I think there are a lot of people who don’t listen to science and don’t understand it. So they’re going to be difficult to sway with the scientifical— scientific arguments.
J.B. HANDLEY: I don’t give a [expletive deleted] about what the MMR said! My kid got six vaccines in one day, and he regressed! You don’t have any science that can show me that the regression wasn’t triggered by the six vaccines. What the parents are saying is, “I went in for a vaccine appointment. My kid got six vaccines, and they regressed.”
We need to ask the question as to why the regression took place, not whether the regression took place, why the regression took place. The only way to do that is to look at that load of vaccines and compare a group of kids or a group of animals who got the load and who didn’t.
NARRATOR: Vaccine critics say many more studies are needed before scientists can rule out side effects like autism— studies of the other vaccines, studies of multiple additives and studies to see if certain children are genetically predisposed to a vaccine reaction. But scientists say undertaking dozens of more studies is not only pointless but also unethical.
SETH MNOOKIN, Assoc. Dir., Science Writing, MIT: We know that vaccines save lives. So you can’t do a traditional study where you take a group of people and say, “Half of them, we’re going to give vaccines to, and half we’ll give a placebo to” because then you’re putting the half that you’re giving the placebo to at risk of very serious diseases.
PAUL OFFIT, M.D., Children’s Hospital of Philadelphia: The hypotheses continue to shift. The first hypothesis, which, you know, people bought into long and hard, is that the combination measles, mumps, rubella, or MMR vaccine, cause autism. Twelve epidemiological studies showed that that wasn’t true.
Then the hypothesis shifted to thimerosal, an ethylmercury-containing preservative that was in vaccines, that’s no longer in vaccines, except for some multi-dose preparations of flu vaccine, that that caused autism. And that clearly has been shown not to be true.
So now this is classic for pseudo-science, is you just keep moving the goalposts. So now the goalpost is, “No, we didn’t mean actually MMR caused autism or thimerosal caused autism, we just meant vaccines in general cause autism.”
NARRATOR: In the vaccine war, two kinds of knowledge compete for the public attention, the collective but dry conclusions of the scientific community and the personal anecdotes of parents.
CYNTHIA CRISTOFANI, M.D., Pediatric Intensivist: It’s a tragedy that there are kids who are unprotected because their parents are choosing not to vaccinate out of fears that are unfounded. The other tragedy is that the kids who have autism, who desperately need better research into why, and more important, what to do about it now— that research isn’t being done, at least to the degree that it should have been, because most of the would-be research— those dollars and hours have been lost.
NARRATOR: The CDC is involved in a long-term study called SEED— the Study to Explore Early Development— to help identify what might put children at risk for autism spectrum disorders and other developmental disabilities. But it’s not clear that such scientific studies will settle the vaccine war. To the contrary, public skepticism of scientific authority seems to be growing, fueled in part by a battleground where ideas fight for public attention, the Internet.
Dr. PAUL OFFIT: I spoke recently at a high school near here. There were about 200 people in the audience, and I asked them how many had gotten the influenza vaccine. And about half raised their hands. Of the half that didn’t raise their hands, they said that they didn’t get it because on YouTube, they saw a Redskins cheerleader say that she had gotten the vaccine and had a so-called dystonic reaction.
NEWSCASTER: [October 19, 2009] She’s the beautiful cheerleader whose heartbreaking story is shocking the nation.
NARRATOR: This clip of Redskins cheerleader Desiree Jennings went viral on the Web after a local Fox News station broke the story. She reported a bizarre neurological reaction to a flu vaccine that caused her to be able only to walk backwards. Her story’s been viewed and shared more than 2.5 million times.
NEWSCASTER: Desiree can run just fine. It’s only when she stops— you see, that’s where the— that’s where the spasms start. Now, you can walk backwards, though.
Dr. PAUL OFFIT: These students who sat in that room were much more likely to believe something they had seen on YouTube from a Washington Redskins cheerleader than they would have believed something that they would have heard from the Centers for Disease Control and Prevention or the American Academy of Pediatrics. That’s a little frightening.
ARTHUR CAPLAN, Ph.D., Center for Bioethics, Univ. of Pennsylvania, 1994-2012: I think the Internet has been fuel on the fire of anti-vaccine fears. There’s plenty of Web sites out there putting out information about people alleging all kinds of complications and problems with vaccines, their own pet theories about what might be dangerous about vaccines. So there are oodles of sources of lousy, dangerous information out there.
NARRATOR: But advocates like Barbara Loe Fisher see the Internet as a democratizing force that has empowered people to challenge medical dogma.
BARBARA LOE FISHER: When I first started this work in the early ‘80s, I had a Selectric typewriter and I had the post office. That’s it. Today, you have access to the library of medicine on the Internet. You can communicate with people all over the world. So it has changed everything.
NARRATOR: In this new world, many parents are no longer willing to take the word of their doctor on faith, or to accept the conclusions of the medical establishment, frustrating public officials charged with protecting the health of the community.
GRETCHEN: I’m the mother of a 2-and-a-half-year-old, and I haven’t done any vaccines at all. And I feel very safe and very comfortable with my decisions.
AUGUSTINE: I’m a midwife, and I’m also the co-leader of the Rogue Valley Holistic Moms Network, which is—
NARRATOR: Ashland’s public health officer, Dr. Jim Shames, has met with parents to talk about their responsibilities for the public health.
Dr. JIM SHAMES: And do you feel that when you say “No, thank you,” that you might be putting anybody else at risk besides your child?
AUGUSTINE: This is the major thing that we’re always up against. Public health officials are looking at the good for all. Mothers are looking at the good for their one child. And that’s very important for them. It’s the most important thing. It’s their world.
Dr. JIM SHAMES: When you make that decision for your child, which you have a right to do, do you think you may be affecting other children?
AUGUSTINE: Do I believe that I’m causing harm by not vaccinating my child? No, I don’t, because if the vaccines work, who am I putting at risk?
Dr. JIM SHAMES: So let’s talk about that. Now, not everybody can get immunized. That child right there is probably too young to get immunized against pertussis. If your child gets pertussis by not getting the vaccine, and your child passes it on to a delicate newborn—
AUGUSTINE: I really don’t believe it. I feel like— first of all, I feel like it would be responsible to then quarantine my child and not expose them to other, you know, potentially fragile populations.
Dr. JIM SHAMES: A lot of diseases are transmitted before you even know you’re sick.
JENNIFER MARGULIS: It’s my responsibility as a parent to keep my child safe, I think, and I don’t think it’s your responsibility to take a vaccine because I might be at the same party with you and you might cough on her. Honestly. I think your job is to protect your own health. And I mean, maybe I sound— I really don’t mean to be sounding selfish in that way.
Dr. JIM SHAMES: There has to be some step beyond just “I take responsibility for me and my kids” because there’s things that happen in the best of intentions that diseases do get transmitted.
NARRATOR: For these Ashland mothers, health is a private affair, not a public responsibility. For them, refusing a vaccine is no more significant than refusing any medication for your child. But ethicists say vaccines are special.
ARTHUR CAPLAN: Vaccines have an odd power that drugs don’t have. If I take a drug, it doesn’t help you. But if I get vaccinated and some others get vaccinated, then you may be benefited by so-called herd immunity.
Dr. PAUL OFFIT: In other words, if a certain percentage of the population is vaccinated, that will stop infections from spreading because most of the people around that child are vaccinated, so therefore, the virus can’t really spread. However, when a critical number of people aren’t vaccinated, when there’s a critical drop in herd immunity, then the viruses can spread. And not only are those children who aren’t vaccinated at risk, but those who can’t be vaccinated are at risk.
NARRATOR: When enough people don’t vaccinate, herd immunity begins to crumble. The first to suffer are vulnerable populations, those who because of age or illness can’t be vaccinated. When Vanessa was 6 weeks old, too young for most vaccines, her only protection was from the herd. Then she came down with a severe cough.
ALVARO FONTAN, Vanessa’s Father: She turned totally blue. She stopped breathing, and we didn’t know what to do to have her breathing back again. I took her outside, you know, bring her back. She wasn’t responding.
NARRATOR: An ambulance brought her to the pediatric ICU in her home town of Portland, Oregon. Fortunately, the intensivist on call that night was Dr. Cynthia Cristofani. This was Vanessa.
Dr. CYNTHIA CRISTOFANI: I look at the video and I keep saying, “Vanessa, take a breath, please” because we knew that a child of that age with an already narrow airway baseline, who’s not inhaling well, could easily lose consciousness from lack of oxygen and perhaps die.
NARRATOR: Dr. Cristofani opened the infant’s airways and sucked copious secretions from her mouth. Vanessa had pertussis, whooping cough. Her status was so dire, a chaplain was brought into the ER.
ALVARO FONTAN: Vanessa was 40 days old when she was diagnosed with whooping cough. So we were probably a week away from having her vaccine for whooping cough. So the only thing that will protect a kid like that will be the herd immunity. And in that case, it failed. I mean, somebody in the community didn’t vaccinate or got Vanessa infected with it.
NARRATOR: Vanessa survived, and the CDC traced her pertussis to an infected student at her brother’s high school.
For the very young and for the very old, scientists say herd immunity matters.
DONNA BRADSHAW-WALTERS, M.D., Pediatrician, Ashland, OR: The more immunity we have in a community, the better it is. Fifty percent is better than nothing, and 100 percent— it’s like building a brick wall around a city and protecting it against an enemy. It’s excellent protection against something entering our community that could cause illness.
NARRATOR: Five years ago, when we last reported on the vaccine war, public health officials were struggling. It was a challenge to explain the importance of herd immunity. But now the political landscape has changed because of the rapidly unfolding measles outbreaks like the one that started at Disneyland in California. The outbreak there, public health officials say, is a sign of poor herd immunity, caused by parents using the personal belief exemption to opt out of the mandatory vaccine schedule required for attending public schools.
SETH MNOOKIN, Assoc. Dir., Science Writing, MIT: There are essentially two types of non-medical exemptions in this country, religious exemptions and personal belief exemptions, The way those two types of exemptions are administered around the country vary widely. In some places, you essentially just need to say, “It is my personal belief that I should not vaccinate my child,” and sign a piece of paper and that’s that.
NARRATOR: Reed Elementary school in Marin County has traditionally made it easy to obtain such exemptions. But now some parents have pushed back, saying that such policies put certain kids at risk. This is 7-year-old Rhett Krawitt. He’s lived with leukemia for most of his young life. He has endured multiple medical procedures and over 50 surgeries. Ninety percent of such cases are eventually fully cured, but the treatment wipes out the immune system, making vaccinations impossible.
CARL KRAWITT, Parent, Marin County, CA: OK, you ready to go, Rhett?
RHETT: I’ve been ready!
JODI KRAWITT, Parent, Marin County, CA: When he was first diagnosed he was pretty much pulled out of society. We avoided highly concentrated groups of people. When we went out, we wore a mask. And we really did limit his exposure. And we just were so excited for the day when he could start kindergarten so he could have that sense of socialization and community and learning.
NARRATOR: A year into remission and back in school, Rhett will soon be healthy enough to be fully vaccinated. But until then, his life depends on herd immunity. And Marin’s high rate of non-medical exemptions therefore puts kids like Rhett at risk.
That’s what this school board meeting is all about.
OFFICIAL: So at this point in the meeting, what we’re going to do is turn it over to public comment.
NARRATOR: Rhett’s family has come to argue that Reed Elementary should bar unvaccinated kids who don’t have legitimate medical exemptions.
CARL KRAWITT: The story isn’t about Rhett anymore. It’s about the hundreds of kids currently with suppressed immune systems that rely on the science of herd immunity. Please eliminate the personal belief exemption as a condition of attendance at Reed.
RHETT KRAWITT: My name is Rhett Krawitt. Leukemia is cancer in my blood—
NARRATOR: Rhett has become a poster child for the pro-vaccine camp, which is now on the offensive, with California politicians considering new legislation to repeal personal belief exemptions.
Dr. RICHARD PAN, California State Senator: My name is Dr. Richard Pan. I’m a state senator representing district 6 in Sacramento. And I really have made extraordinary efforts to be sure that our children are safe—
NARRATOR: And there are similar plans in other states.
REPORTER: What do you want the board to do?
RHETT KRAWITT: To make sure everybody gets vaccinated.
BARBARA LOE FISHER, Pres., National Vaccine Info. Ctr.: Have you talked to your pediatrician?
NARRATOR: But vaccine watchdogs like Barbara Loe Fisher oppose such legislative attempts to limit parental choice, turning again to the Internet.
BARBARA LOE FISHER: [Web video, January 28] The battle lines are clearly drawn. Now Americans have a choice to make. Will we stand up and fight to protect our freedom to make voluntary decisions about which vaccines we buy and use, or will we permit liability free drug companies and government health officials to take that freedom from us?
NARRATOR: Jennifer Margulis has also joined the fight, testifying against a new Oregon bill to ban personal belief exemptions.
JENNIFER MARGULIS, Parent, Ashland, OR: For me, this is a debate about freedom and parental choice. Oregon should be educating parents about vaccines and vaccine safety. There is no place for forced vaccination in a free society. Thank you.
NARRATOR: And some politicians are being asked to weigh in on this divisive issue.
Gov. CHRIS CHRISTIE (R), New Jersey: Parents need to have some measure of choice in things, as well. So that’s the balance that the government has to decide.
REPORTER: Did you really just say that you think most vaccines in this country should be, quote, “voluntary”?
Sen. RAND PAUL (R), Kentucky: The state doesn’t own your children. Parents own the children. And it is an issue of freedom.
NEWSCASTER: —Hillary Clinton tweeting, “The science is clear. The earth is round, the sky is blue and vaccines work,” adding “grandmothers know best.’
ARTHUR CAPLAN, Ph.D., Center for Bioethics, Univ. of Pennsylvania, 1994-2012: Parents don’t have unlimited rights with respect to the welfare of their children. You can’t put them at risk of fatal disease. You can’t put them at risk of devastating disability.
You know, the ethics isn’t just on the side of the critics. The ethics is also on the side of those who say, “Do good in the name of children. Do good in the name of public health.”
NARRATOR: One thing both sides can agree on, there’s a lot at stake in the vaccine war— on the one hand, the fear that American communities will be exposed to serious diseases, on the other, something equally compelling, every parent’s wish to do what’s best for her child.
THE VACCINE WAR
PRODUCED AND DIRECTED BY Jon Palfreman and Kate McMahon
WRITTEN BY Jon Palfreman
EDITORS Raoul Rosenberg Nathan Hendrie
DIRECTOR OF PHOTOGRAPHY Mark Rublee
EDITORIAL PRODUCER Tom Delbanco, MD
GRAPHIC ANIMATION Mark Rublee
NARRATED BY Will Lyman
ORIGINAL MUSIC John E. Low
ADDITIONAL MUSIC Justin Samaha
ADDITIONAL CAMERA Jack Bromiley Brian Dowley
ADDITIONAL SOUND Jack Combs Steve Bores Kevin Crawford
ONLINE EDITOR/ COLORIST Jim Ferguson
SOUND MIX Jim Sullivan
ADDITIONAL RESEARCH Michaela Santen
TRANSCRIBERS Johanna Kovitz Karen Weitzel Shelli Kennedy
ADDITIONAL VOICE-OVER Robin Parmelee Charles Linshaw
SPECIAL THANKS Center for Applied Social Research, University of Oklahoma Amy and Paul Murphy Brenna and Dan Weatherby Jaime Rublee SOU Schneider Children’s Center OHSU-OIT Paramedic Program Suzann Schmidt Scripps Memorial Hospital Encinitas Doylestown Hospital YMCA Ashland, OR Mary’s Woods San Diego International Airport Group Health Cooperative, Seattle Skolen på Islands Brygge
ARCHIVAL MATERIAL ABCNEWS VideoSource CNN Image Source BBC ITN WETA March of Dimes Foundation The Lancet FOX 5 News, Fox Television Stations, Inc. First Signs CDC Pfizer, Inc. Oregon Legislative Media
FOR FRONTLINE
PRODUCTION MANAGER Megan McGough Christian
ON-AIR PROMOTION PRODUCER Missy Frederick
ON-AIR PROMOTION EDITOR Barry Clegg
ASSISTANT EDITORS Eric P. Gulliver Lindsey Rundell
POST PRODUCTION ASSISTANT Kenzie Audette
FOR WGBH OUTPOST
DIRECTOR OF POST PRODUCTION Chris Fournelle
SENIOR DIRECTOR PRODUCTION TECHNOLOGY Tim Mangini
SERIES MUSIC Mason Daring Martin Brody
DIRECTOR OF AUDIENCE DEVELOPMENT Pamela Johnston
PUBLICITY ACCOUNT MANAGER Patrice Taddonio
DIGITAL COMMUNITY SPECIALIST Shauna Stuart
SECRETARY Christopher Kelleher
EDITORIAL SECRETARIES Sophie Gayter Amy Gaines
RECORDS MANAGER John Campopiano
CONTENT MANAGER Lisa Palone
LEGAL Eric Brass Jay Fialkov Janice Flood
SENIOR CONTRACTS MANAGER Gianna DeGiulio
UNIT MANAGER Sue Tufts
DIRECTOR OF BUSINESS Tobee Phipps
PODCAST PRODUCER/REPORTER Lu Olkowski
DIGITAL RESEARCH ASSISTANT Priyanka Boghani
DIGITAL ASSOCIATE PRODUCER Jason Breslow
DIGITAL VIDEO PRODUCER Michelle Mizner
SENIOR DIGITAL REPORTER Sarah Childress
INTERACTIVE EDITOR Chris Amico
MANAGING EDITOR, DIGITAL Sarah Moughty
POST COORDINATING PRODUCER Robin Parmelee
SERIES COORDINATING PRODUCER Carla Borras
SPECIAL COUNSEL Dale Cohen
SENIOR EDITORIAL CONSULTANT Louis Wiley Jr.
SERIES SENIOR EDITOR Andrew Metz
MANAGING DIRECTOR Jim Bracciale
DEPUTY EXECUTIVE PRODUCER Raney Aronson-Rath
EXECUTIVE PRODUCER David Fanning
A FRONTLINE production with the Palfreman Film Group in association with Kate McMahon Productions, LLC
©2010, 2015 WGBH EDUCATIONAL FOUNDATION ALL RIGHTS RESERVED
FRONTLINE is a production of WGBH/Boston, which is solely responsible for its content.
Explore
Policies
Teacher Center
Funding for FRONTLINE is provided through the support of PBS viewers and by the Corporation for Public Broadcasting, with major support from Ford Foundation. Additional funding is provided the Abrams Foundation, Park Foundation, John D. and Catherine T. MacArthur Foundation, Heising-Simons Foundation, and the FRONTLINE Trust, with major support from Jon and Jo Ann Hagler on behalf of the Jon L. Hagler Foundation, and additional support from Koo and Patricia Yuen. FRONTLINE is a registered trademark of WGBH Educational Foundation. Web Site Copyright ©1995-2025 WGBH Educational Foundation. PBS is a 501(c)(3) not-for-profit organization.