Rhode Island PBS Weekly 6/23/2024
Season 5 Episode 25 | 26m 39sVideo has Closed Captions
Steph Machado reports on the warehousing of children in a local psychiatric hospital.
Steph Machado reports on the warehousing of Rhode Island’s most vulnerable children in a psychiatric hospital. Producer Isabella Jibilian explores the medical treatments for women going through menopause. Michelle San Miguel and WPRI 12’s politics editor Ted Nesi discuss the rise of the House Speaker and why Lifespan has a new name.
Problems playing video? | Closed Captioning Feedback
Problems playing video? | Closed Captioning Feedback
Rhode Island PBS Weekly is a local public television program presented by Ocean State Media
Rhode Island PBS Weekly 6/23/2024
Season 5 Episode 25 | 26m 39sVideo has Closed Captions
Steph Machado reports on the warehousing of Rhode Island’s most vulnerable children in a psychiatric hospital. Producer Isabella Jibilian explores the medical treatments for women going through menopause. Michelle San Miguel and WPRI 12’s politics editor Ted Nesi discuss the rise of the House Speaker and why Lifespan has a new name.
Problems playing video? | Closed Captioning Feedback
How to Watch Rhode Island PBS Weekly
Rhode Island PBS Weekly is available to stream on pbs.org and the free PBS App, available on iPhone, Apple TV, Android TV, Android smartphones, Amazon Fire TV, Amazon Fire Tablet, Roku, Samsung Smart TV, and Vizio.
Providing Support for PBS.org
Learn Moreabout PBS online sponsorship(gentle bright music) - [Pamela] Tonight: the warehousing of Rhode Island's children.
- It is an appalling failure.
Instead of living the normal life of a kid, you're in a locked room in a psychiatric hospital.
- [Michelle] Then, why have so many women been suffering silently?
- They've been miserable for so long, for no good reason.
- [Pamela] And we look at the expanded partnership of Lifespan and Brown University with Ted Nesi.
(bright inquisitive music) (bright inquisitive music continues) Good evening.
Welcome to "Rhode Island PBS Weekly."
I'm Pamela Watts.
- And I'm Michelle San Miguel.
We begin tonight with shocking revelations about what happened to some of Rhode Island's most vulnerable children.
- In May, the federal government accused state officials of warehousing children in a psychiatric hospital for months on end.
If local officials can't turn the situation around, the Department of Justice will likely bring a lawsuit against Rhode Island.
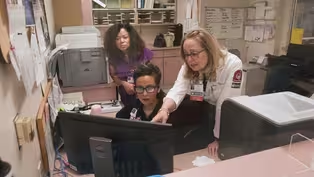
Our contributor, Steph Machado, recently talked to several people at the center of this disturbing case.
- This is Rachel.
She was about three years old here.
- [Steph] For years, Mary McDonough has spent more time visiting her daughter than living with her.
- It was very disturbing to be away from her.
- [Steph] 15-year-old Rachel was diagnosed with autism when she was six.
- She was one of those that was hard to diagnose.
She was very social, cracked jokes, you know, she talked a lot, she gabbed, and she didn't present as a typical child with autism.
- [Steph] Her mental health and behavioral problems started as young as three years old and only got worse as she got older.
- As the years went on, she became very aggressive.
She was doing a lot of self-injury, headbanging, biting herself.
She started throwing things and breaking things and it got to be, you know, when she was really in a rage, we had this thick, heavy wooden table and she would like lift it up and throw it.
You know, she seemed to have like this strength that was incredible.
- That's how Rachel landed at Bradley Hospital for the first time back in 2017 when she was nine.
It's the only psychiatric hospital for children in Rhode Island.
When you got to Bradley, how long did you think she was gonna stay there?
- Well, so when you walk into Bradley into the admission section, there's a sign that says how long your child's gonna be there, and it's 7 to 10 days.
So that was my understanding, 7 to 10 days.
- [Steph] The reality was much different.
- She was in and out of Bradley for lengthy stays.
I'm talking, you know, six to nine month stays.
- [Steph] Mary says Rachel spent more than 1,000 nights at Bradley Hospital, over a dozen admissions in five years.
- She essentially lived there.
She was there more than she was home.
When she was able to come home, it was just the same thing, you know, it didn't seem like anything was working for her.
And so there was no services because there wasn't any available.
And we tried.
We tried to keep her home.
We did it for as long as we can, but as she got bigger, you know, she was throwing me against the wall and she was pushing me onto the floor.
- [Steph] Eventually, her parents were confronted with a difficult choice: to discharge Rachel to a residential treatment center rather than continuing the cycle of repeat hospitalizations.
- To find a residential was, you know, what they told us was just turning out to be impossible.
There was nothing in Rhode Island available.
There was no girls' residentials.
And so they started, you know, towards the end, looking like all over the United States.
That was just one of those things that I had a hard time with because how can you mother your child in California?
- [Steph] Mary says it took a year for the Department of Children, Youth & Families, or DCYF, to find a spot for Rachel at a residential facility in Massachusetts.
For most of that time, she languished at Bradley.
- As it turns out that Bradley Hospital is just like a nursing home for children waiting for residential placement.
- It is an appalling failure.
- Rhode Island's U.S. Attorney Zachary Cunha says the Department of Justice started investigating the situation at Bradley in 2022.
- We looked at a time period between 2017 and 2022, and in that time we found there were 527 kids who were housed longer than they should have been at Bradley.
The idea that you're basically, instead of living the normal life of a kid, you're in a locked room in a psychiatric hospital.
The potential consequences of that are terrible.
- [Steph] Cunha sent his findings to state officials in May, accusing the state of violating the civil rights of hundreds of children, some of whom were at Bradley for more than a year.
- The Supreme Court has said for over 20 years going on 30, that basically individuals with disabilities need to be treated in the least-confining setting appropriate to their condition.
So you have kids who require hospitalization 'cause they're in crisis and they need to be stabilized, but when that crisis is over, they're supposed to be cared for in a less restrictive setting.
And that's what's not happening here and that's what our case is about fundamentally.
- [Steph] Cunha says he does not place blame on Bradley Hospital.
- Bradley Hospital definitely did identify some of these issues here.
They flagged some of these cases to DCYF.
In fact of the problem here is that you had professionals at Bradley Hospital telling DCYF, "These kids are ready to go.
They're ready to move on from our care."
And DCYF failed to place them in less restrictive contexts.
- Both the DCYF director, Ashley Deckert, and Governor Dan McKee declined to be interviewed for this report about what they are doing to try and solve this crisis.
A spokesperson says the state is in confidential talks with the Department of Justice and it would be premature to talk about next steps.
- The state has reached out to us, we've begun discussions.
We have heard and seen things in the course of our investigation that suggest that DCYF is aware of this issue and is amenable to making change.
- In a one-page letter responding to Cunha on May 22nd, Director Deckert said, quote, "Ensuring the safety and wellbeing of Rhode Island's children is DCYF's top priority," while also blaming the issue on, quote, "nationwide mental health staffing challenges."
- If the state needs to revise how it conducts these programs structurally, if it needs to revisit how it does discharge planning, whatever the cause, the state needs to fix it.
- So the options are, you come to some sort of settlement or agreement with the state or you sue?
- Basically, yes.
I am hopeful.
I am always hopeful.
It's always in everyone's best interest to try and resolve issues without litigation.
The goal here is to get these kids the care they need, not to wind up in court for many years, but we're gonna see where these discussions go.
- In Rhode Island, there is not meaningful discharge planning going on because there are not meaningful supports in the community to go to.
- Morna Murray, the executive director of Disability Rights Rhode Island, was not surprised by the DOJ's findings.
- There is a dearth of community services available.
There are not enough providers, there is not enough money being spent on community-based services.
And while we're talking about community-based services, just to demystify that word, it's just services that are available to children and families where they live rather than having to go to a residential setting, which is the, you know, option of last resort, when we're talking about vulnerable kids.
They don't belong in hospitals.
- [Steph] DCYF says they contract with residential facilities, group homes, and in-home services, all options for children being discharged from Bradley.
But the DOJ says there are not nearly enough and the state has pulled children out of the only psychiatric residential facility in the state, St. Mary's Home in North Providence, amid allegations of abuse, neglect, and dysfunction.
The use of residential facilities is a hotly-debated topic in the child welfare world.
- There's all kinds of, not only anecdotal evidence, but hard evidence across the country that these kinds of residential settings are harmful for children.
Far from being an answer, they actually exacerbate distress and other behavioral health challenges that children are experiencing.
- [Steph] Currently, 76 children in DCYF's care are placed out of state, including Rachel McDonough, because of the lack of facilities here.
Responding to the need, two years ago, lawmakers approved $45 million for a 16-bed residential facility for girls.
Construction is set to begin this summer in Exeter.
- Adding more beds so that you can long-term institutionalize more kids who can be adequately cared for in the community, that's not the solution.
That's exacerbating the size of the problem.
- We would advocate for taking some of the money, a significant portion of the money that's going towards residential beds, and putting that towards community services because not only are community services more effective, more compassionate, creating more connections for children, which is what they need, but they're far cheaper, far less expensive.
They are a fraction of what residential care costs.
- One of those options is called therapeutic foster care, where foster parents are trained and paid to care for children with special needs.
The DOJ found that the state cut the pay to those foster parents in 2020, which, over time, led to fewer families being available that could have taken in children waiting to be discharged from Bradley.
- Of course we're outraged by that and we can't understand that.
At the same time, state governments are constantly robbing Peter to pay Paul, - [Steph] In the most recent legislative session, lawmakers funneled millions of additional dollars to DCYF, including for foster care and for workforce development so mental health providers can hire more staff.
- My ideal scenario would be, Rachel would be home with her family, I would have staff here to take care of her.
- And does that scenario not exist?
- It does not.
- [Steph] Mary McDonough says Rachel is doing better at the residential treatment facility in Massachusetts where she also receives rigorous schooling after missing so much education while living in the hospital.
But she's only allowed to see her parents for short visits.
- Well, we want her home, you know, we want her back home.
If services become available where we can take her home, that would be great.
But the school systems here, even the private schools just have been, in the past, unable to deal with her so she didn't really get an education.
She's missed most of her childhood.
- Do you believe the state of Rhode Island has failed Rachel?
- The state of Rhode Island has failed her miserably, has failed our whole family.
- The president of Bradley Hospital, Dr. Henry Sachs, says the DOJ's findings are consistent with what's happening at the hospital.
- And Dr. Sachs maintains that Bradley Hospital has been pushing for DCYF to find solutions so they can discharge children faster.
You can read more of what Dr. Sachs had to say in "The Boston Globe" at globe.com/ri.
Next up: for women going through menopause, the life chapter is more than a passing phase.
Many suffer a myriad of debilitating medical issues for a decade or more.
Tonight, we take a look at growing interest in this area of women's health, exploring how old and new research is shaping the medical care women receive.
Producer Isabella Jibilian has the story.
- It was rage for no reason.
I felt bile coming outta my mouth and didn't feel any way to control it.
The only one I wasn't mad at was the dog.
- [Isabella] Artist Tanya Glover was 45 years old when she started noticing symptoms that she couldn't explain.
- The anxiety big time.
That was the worst one.
The night sweats, the irregular periods, the heavy periods.
I just felt like I was kind of losing it a little bit.
And a friend of mine said something about perimenopause.
I'm like, "What is that?"
- It's a familiar story for Dr. Mary Jane Minkin.
- Menopausal symptoms, perimenopausal symptoms, can be extraordinarily disruptive to women.
- [Isabella] Those symptoms can include: increased anxiety, hot flashes, migraines, insomnia, vaginal dryness, and changes in sexual desire.
And Dr. Minkin says, all too often, they aren't taken seriously.
- I just feel horrible for so many of these women who come in and they've been miserable for so long for no good reason.
We have some great therapies for them so that people can lead totally normal lives.
- [Isabella] Those therapies are going unused because traditional treatment, hormone replacement therapy, developed a bad reputation in 2002.
Dr. Minkin says a study called the Women's Health Initiative, or WHI, changed everything.
- I remember where I was when JFK was shot, I remember where I was at 9/11, and I remember where I was on July 9th, 2002.
- [Isabella] The hormone estrogen has been successfully used to treat menopause symptoms since the '40s.
- [Dr. Minkin] And many people started viewing estrogen as sort of a fountain of youth.
- Scientists hypothesized that it could help with other diseases.
- Dr. Grant prescribed Premarin.
- [Isabella] And in the '90s it was put to the test.
- The birth of the Women's Health initiative was to study, does estrogen really help prevent heart disease?
- [Isabella] About 27,000 women were divided into two groups.
Women who had hysterectomies were given estrogen or a placebo, women with uterus were given estrogen and a synthetic progesterone or a placebo.
- It was supposed to go on for over 10 years.
Yes.
- Dr. Renee Eger is the director of the menopause program at Women & Infants Hospital.
- After five years, there was noted to be a statistically-increased risk of breast cancer in the women who took the estrogen plus the synthetic progesterone.
- That basically stopped the study dead in its tracks.
Indeed, I got more calls that day than ever before or ever after (chuckles) of everybody who's terrified, you know, "I'm taking this estrogen, I'm gonna get breast cancer and die."
- That study made it onto the front page of "The New York Times," it was the topic of talk shows.
The number of prescriptions for hormone replacement therapy decreased by 85%.
Those numbers have not rebounded.
- [Isabella] Today, Tanya Glover takes an anti-anxiety medication for her menopause-related depression and anxiety.
- Wait for me.
It's taken the edge off.
(chuckles) That's it though.
It's still there.
I probably couldn't do a job, a regular job.
I don't think I could handle it.
And that's not an option for a lot of people.
- Did you ever consider hormone therapy?
- I considered it.
My doctor told me most insurances don't cover it and it's pretty expensive.
And you know, you hear about the cancer risks and I don't know who to believe.
- [Isabella] Who and what to believe about the WHI's findings has been the question for the last 20+ years.
- The actual increased numbers of breast cancer was only 8 women out of every 10,000 women so from a clinical standpoint, it was questionable whether that was actually significant.
But from a statistical standpoint, the study was so large that they had to conclude that there was statistical significance.
- [Isabella] Plus, the women who were studied weren't your standard candidates for hormone therapy.
- The average age of women enrolled in the WHI was 63.
The average age of women going through menopause is 51 so you had these women who were way post menopause.
Oh, by the way, 20% of the women were between 70 and 79 in the WHI.
And do I enroll a lot of women or start women in their 70s in general on estrogen?
Not really.
- [Isabella] In May, a study published in "The Journal of the American Medical Association" took another look at data from the WHI and other studies and found that hormones were safe for many women under 60 to take.
- The hormone replacement therapy of 2024 looks very different than it did back in 2002.
We learned that the use of probably a synthetic progestogen does likely increase a woman's risk of breast cancer.
And we've changed the way in which we deliver our estrogen.
We used to deliver it orally and now it can be delivered through the skin and there's increased safety associated with delivering the medication that way.
- How safe do you consider hormone therapy to be?
- For women who are at low risk and appropriate candidates for hormone therapy, hormone therapy is very safe when you look at the risks versus the potential benefits associated with it.
We no longer tell women that they absolutely are or are not candidates for hormone therapy, but rather have individualized discussions with patients and take a look at their past medical history.
I think it's also important that people understand that there are alternatives to hormone therapy because hormone therapy isn't necessarily the right choice for every woman.
- Are most providers prepared to have this kind of in-depth conversation?
- I think a lot of that depends on when an individual completed their residency.
- [Isabella] Dr. Minkin says that's because the WHI changed the way doctors are trained.
- Because women stopped using estrogen in droves, most programs training residents in OB-GYN and some other specialties basically stopped teaching how to manage menopause.
- So they didn't think they had any good treatment options and therefore they stopped teaching about menopause altogether.
- Exactly.
Even as of last year, 70% of the OB-GYN programs in the United States were not teaching menopause management.
(Dr. Eger knocks) - [Dr. Eger] Hi, it's Dr. Eger.
- [Isabella] And many patients don't believe their symptoms can be treated safely.
- The data bears out that most women who are having hot flashes are actually not seeking medical attention.
- [Isabella] But there are signs that change is happening.
- This is a big year for menopause, by the way.
Big year.
Just a little over a year ago, it was the cover story of "The New York Times" Sunday magazine and the title was: Women Have Been Misled About Menopause.
And this started a revolution.
- Why is such a critical part of women's health being ignored?
- This is a normal part of the perimenopause-to-menopause transition.
- Menopause, on page 242, is mandatory, suffering is not.
- [Isabella] On social media.
- Good morning, menoverse.
Okay.
- Do your periods just stop when you enter menopause?
- Can you tell me what menopause is?
- When a woman no longer experiences their period?
I don't know.
Is that it?
- Good for you.
- [Isabella] And in government.
In March, President Biden requested $12 billion for women's health research, noting menopause as a particular area of interest.
(bright music) - [Advertiser] This is a hot flash.
- [Isabella] And a new non-hormonal drug - This is a hot flash.
- has become available and was advertised during the past Super Bowl.
- [Advertiser] This is a not flash.
- As for Tanya Glover, it's been a long, turbulent phase of life.
How many years has it been now?
- At least 10.
- Of perimenopause?
- I haven't had a period since last March, so I'm like a week or two away from full-blown menopause.
- How does that feel?
- I don't wanna jinx it, (laughs) but it feels like relief is right around the corner.
I need that.
- Finally tonight, on this episode of "Weekly Insight," Michelle and WPRI 12's politics editor Ted Nesi discussed the rise of House speaker Joe Shekarchi and why the state's biggest hospital group has a new name.
- Ted, welcome back.
It's good to see you.
So we have big news to share in the world of healthcare.
The largest hospital group here in Rhode Island, Lifespan, announced a plans to form a deeper relationship with Brown University.
Lots of layers to this, but I think the first thing people will notice is this comes with a name change.
- Yes, so Lifespan, just to remind everyone, is the parent of Rhode Island, Miriam, Newport, and Bradley Hospitals, and they will be getting a new name, Brown University Health, and that's gonna start to roll out this fall or winter.
- To be clear, this does not mean there's a merger happening.
Brown is not taking over Lifespan.
- Correct.
- None of the sort.
But really this is adding to what's been a longstanding relationship between the two organizations.
- Right, so Rhode Island Hospital has been the prime teaching hospital for Brown's Medical School since the Medical School was founded in the 1970s.
But this really flows out, Michelle, of the turmoil around the future of the hospital sector in Rhode Island that we've seen for the last decade, decade plus.
We've seen multiple failed merger attempts, the Lifespan-Care New England merger, the Brigham takeover of Care New England that didn't go through.
And I think Brown, over time, came to the realization that they really had to be central to any solution to all of this.
And so what you see here is, along with Brown lending its name to Lifespan going forward in the hospitals, they're gonna put a lot of money into Lifespan, $150 million over the next seven years, which is a shot in the arm for Lifespan, which has been unable to invest as much as they needed to in, you know, in technology and facilities in all of that.
So I think you see here, Brown sort of acknowledging that they need to use their deep pockets to try to stabilize what's a very important partner to them.
- I think most people want to know, ultimately, what does this mean for the quality of care?
For those who maybe are not satisfied with the care they're receiving there, can they expect an improvement?
And for those who are, will the status quo remain?
- Well, I put that question to the CEO of Lifespan, John Fernandez, after the press conference, he said he thinks, for the average patient, this is really just a name change, they're gonna see a different name on the door, different name on the letters they get from their doctor.
He does hope, he says, that, over time, patients will notice improvements, again, from the investments from the money Brown is providing and perhaps from the ability to kind of recruit more clinicians, more top-notch doctors, and all of the effects of that.
But we'll have to see if it pays off as much as they're hoping today.
- Right.
We'll keep tracking that.
Let's also discuss the end of the General Assembly session.
Of course, hundreds of bills passed.
One of the top ones that we've been discussing was a priority for House Speaker Joe Shekarchi expanding accessory dwelling units, also known as ADUs.
And for many people they have viewed this as, really, the way to solve the housing crisis in Rhode Island.
But it passed, but not before it was met with very strong resistance in the State Senate.
- Yes, and people might remember that last year this bill failed, even though the House speaker, the most powerful lawmaker on Smith Hill, wanted it.
He didn't get it last year.
He got it through this year, but it was a narrow vote in the Senate, Michelle, which, as you say, I think speaks to the concern.
And frankly, the opponents seemed to have the same concerns that the supporters hope is a positive, which is, this could lead to a lot of additional housing units, people turning maybe a garage, above your garage, you know, becoming a spare bedroom with a kitchenette and a little bathroom, or maybe an old shed or an unused bit of your backyard could become something.
Shekarchi, and people who think like him, say that's a positive.
That's what Rhode Island needs as one part of the solution to the housing crisis, to, you know, lots of infill housing, but opponents worry about will it change the character of a neighborhood, will lead to too many rentals in places they wouldn't usually be and all of that.
We have seen California adopt this in recent years, another places with a big housing crisis, and they have seen a lot of units added.
So we're now gonna have to see how it's actually, how the average Rhode Islander, you know, takes this law and what do they build with it.
- Sure, and I think, too, maybe people who were considering moving out of Rhode Island, feeling like they were being priced out may decide to stay.
- Well, and that's part of what they're really hoping for here, Michelle, is it's one more piece that will allow for some more churn in the housing market.
Let people, a family that's growing that needs a bigger house, make it easier for them to find a place.
Maybe someone who wants to downsize can find a smaller place to live.
Young people needing just a one-bedroom apartment that they can afford, maybe more of that.
So you know, we will see if it works.
- Thanks so much, Ted.
Appreciate it.
- Good to be here.
- And that's our broadcast this evening.
I'm Pamela Watts.
- I'm Michelle San Miguel.
We'll be back next week with another edition of "Rhode Island PBS Weekly."
Until then, please follow us on Facebook and X and visit us online to see all of our stories and past episodes at ripbs.org/weekly or listen to our podcast on your favorite streaming platform.
Goodnight.
(gentle music) (gentle music continues) (gentle music continues) (gentle music continues)
Video has Closed Captions
Clip: S5 Ep25 | 11m 23s | Steph Machado reports on the warehousing of children in a local psychiatric hospital. (11m 23s)
Video has Closed Captions
Clip: S5 Ep25 | 3m 59s | Rhode Island’s largest hospital group, Lifespan, will be renamed Brown University Health. (3m 59s)
Video has Closed Captions
Clip: S5 Ep25 | 10m 17s | Why menopause symptoms go untreated. (10m 17s)
Providing Support for PBS.org
Learn Moreabout PBS online sponsorship
- News and Public Affairs

Top journalists deliver compelling original analysis of the hour's headlines.

- News and Public Affairs

FRONTLINE is investigative journalism that questions, explains and changes our world.












Support for PBS provided by:
Rhode Island PBS Weekly is a local public television program presented by Ocean State Media