Call The Doctor
Lyme Disease: What You Need to Know
Season 33 Episode 16 | 25m 20sVideo has Closed Captions
The CDC estimates that 35,000 cases of Lyme Disease get reported each year
The Centers for Disease Control estimates that 35,000 cases of Lyme Disease get reported each year. Symptoms include a flat circular rash anywhere on the body, joint pain, headaches, and fever. In 2018, the highest number of confirmed cases, was reported in Pennsylvania.
Problems playing video? | Closed Captioning Feedback
Problems playing video? | Closed Captioning Feedback
Call The Doctor is a local public television program presented by WVIA
Call The Doctor
Lyme Disease: What You Need to Know
Season 33 Episode 16 | 25m 20sVideo has Closed Captions
The Centers for Disease Control estimates that 35,000 cases of Lyme Disease get reported each year. Symptoms include a flat circular rash anywhere on the body, joint pain, headaches, and fever. In 2018, the highest number of confirmed cases, was reported in Pennsylvania.
Problems playing video? | Closed Captioning Feedback
How to Watch Call The Doctor
Call The Doctor is available to stream on pbs.org and the free PBS App, available on iPhone, Apple TV, Android TV, Android smartphones, Amazon Fire TV, Amazon Fire Tablet, Roku, Samsung Smart TV, and Vizio.
Providing Support for PBS.org
Learn Moreabout PBS online sponsorship- "Lyme Disease: What You Need to Know," coming up next on "Call the Doctor."
(bright music) - [Announcer] The region's premier medical information program, "Call the Doctor."
(bright music) - Lyme disease is an infectious disease that is caused by the bite of a blacklegged tick, also known as the deer tick, that carries the bacteria that causes the Lyme infection.
The Centers for Disease Control estimates that 35,000 cases of the disease get reported each year.
People who live or spend time in wooded or grassy areas are more likely to get this illness.
Pets that have been in a wooded area also have a high risk of contracting the disease.
The longer the tick remains attached to your skin, the greater the risk of getting infected.
Symptoms include a flat, circular rash anywhere on the body, joint pain, headaches, and fever.
Roughly 10% of people treated for Lyme infection do not recover from the disease.
Antibiotics, which can be administered both orally and intravenously, are used to treat the illness.
In 2018, the highest number of confirmed cases, 7,920, was reported in Pennsylvania.
"Lyme Disease: What You Need to Know," now on "Call the Doctor."
Welcome to "Call the Doctor" here on WVIA.
I'm Paola Giangiacomo.
Tonight, our topic is Lyme disease.
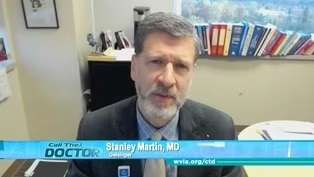
Joining us on the panel, Dr. Stanley Martin.
He is a board certified and fellowship trained specialist in infectious diseases at Geisinger.
Dr. Jodi Lenko, she is the Vice Chair, Department of Medicine, at Lehigh Valley Hospital in Hazleton.
And Nicole Chinnici, she's the director of the Dr. Jane Huffman Wildlife Genetics Institute at East Stroudsburg University.
And I would like to remind our viewers that you can participate in the conversation at wvia.org/ctd.
You can also submit your questions for future shows by emailing ctd@wvia.org or using the hashtag #wviactd.
And be sure to check our website for a listing of future programs, and watch "Call the Doctor" episodes any time on the WVIA app or on wvia.org.
Now, we'll begin our discussion.
Thank you all for joining us for this virtual program.
Let's start off with Dr. Lenko.
If someone finds a tick on their body, should they immediately become concerned?
- The most important thing to do if you find a tick on your body is to try to safely remove it as quickly as possible.
So the way you do that is you try to grab just below the head and try to get the fangs of the tick, the teeth out of the body.
And then clean it with soap and water.
That's the most important thing to do almost immediately.
And the next thing to do after that is to try to figure out if you know how long the tip was on you.
If you know, for instance, that it's on your leg and you know for a fact that it was not on you this morning when you took a shower, and a couple hours later you found a tick and it's not engorged, you have less reason to be concerned.
If you're not sure or you don't know, or if you think the tick might've been on you for more than a day, that's the best time to call your doctor to get the next steps for advice.
- So Dr. Martin, how long does an infected tick have to be on you before you become infected?
- Well for Lyme disease, the tick usually has to be attached for at least a good 24 hours, if not even longer in order for the bacteria, which is the cause of Lyme disease, to make its way out of the tick and into the host.
- And Nicole, you test ticks.
So if someone finds a tick, should they send it in to get tested to see if it's infected with Lyme disease?
- Yes.
So ticklab.org is our website.
And we're funded through the Department of Health, so Pennsylvania residents can receive free tick testing.
And the important thing about tick testing is we can also determine how long that tick was attached.
So we'll let you know estimated time so that you can understand your risks.
So if the tick is a carrier of Lyme disease, you'll know if it's longer than that 24-hour period, if you have a greater risk of that transmission to have occurred.
- So how should someone remove a tick from themselves?
Like, should they use tweezers?
Should they do it very slowly, carefully?
Or just rip it right off?
Nicole?
- Yeah, using a tweezer is the best method.
You don't wanna use anything such as petroleum jelly or alcohol, anything where the tick would back out easily, because as mentioned, the bacteria is activated in the mid-gut of the tick and transmits through the salivary glands.
So the tick backs out easy, there's a chance that it could push that bacteria or other viruses into you faster.
So using a tweezer or a tick removal tool that will scoop the tick right up and out, grabbing close to the mouth parts in the skin is the best method.
- Okay, and Dr. Lenko, what are the signs and symptoms that you might have Lyme disease?
What should you look for?
- Yeah, so I think it's also important to note that the signs and symptoms usually start a few days to up to a month after the tick bite, and they're not always immediate.
So oftentimes patients will come to me with a tick on them and saying it's red right around the tick bite.
I have the rash.
And that's not really the rash.
That's usually more of a local reaction to the bite itself.
So oftentimes the symptoms that we're looking for with true Lyme disease typically happen on average about seven days later, but can happen to as late as up to 30 days later.
And that often includes fatigue, sometimes headaches, some fevers, chills, sometimes joint aches and muscle aches.
There's a variety of symptoms.
And unfortunately, there's not a lot of specific symptoms, so they overlap with a lot of other things, flu-like illnesses and other things that could be going on.
So sometimes it's tricky to pinpoint the symptoms.
- It's interesting, those symptoms you just described sound like COVID vaccine symptoms.
That's how I felt after my second shot, right?
- Yes, there's a lot of overlap with flu-like illnesses.
And unfortunately, being a primary care doctor, we deal with fatigue all the time.
So this is something that is important to try to tease out.
And where we live in Pennsylvania, as Dr. Martin will probably attest, is that we're endemic to Lyme disease.
There's ticks with Lyme disease all around us.
So it is tricky to try to, you know, to figure out when we need to be worried.
It's a little easier when they know they had a tick bite.
It's a little bit harder when the history is not there.
- Sure, so if left untreated, Dr. Martin, are there later signs of Lyme disease?
- So yes.
Usually if the disease continues to progress, if it's not treated, then that's when people tend to get the very recalcitrant arthritis.
So they start to get more pain and swelling in the joints.
The knee tends to be the most common joint affected by this.
And we can see that it tends to migrate around.
So one joint might be affected, then another joint might be affected.
And that can persist sometimes even for months.
Other manifestations can happen, but are more rare later on in the disease course, although they sometimes can happen early as well.
And that includes what we might call meningitis, where you get kind of inflammation in the brain or the lining of the brain.
And even carditis, which is inflammation of the heart.
Both of those are fairly uncommon, particularly the manifestations with the heart.
That is very rare indeed, but it can happen.
- And Lyme disease can spread to other parts of the body.
Is that right, Dr. Martin?
- Well, again, we're talking about places like the brain, spinal cord, the heart, the joints.
Yeah, in that sense, it can spread to other parts of the body.
- Wow.
That's serious.
And Nicole, you actually not only test ticks, but you test illnesses associated with ticks.
So tell me more about the kinds of things that you test.
- So ticks can carry a plethora of different illnesses.
They vary from viruses like Powassan virus, so we'll test for Powassan virus.
Protozoal, like Babesiosis, so we test for different types of Babesiosis species that ticks can transmit.
Anaplasmosis, ehrlichiosis.
So there's a bunch of different pathogens that these ticks can transmit to us.
And we track all those illnesses on our website so that physicians can utilize that information to help with guiding treatment and diagnosis in addition to testing that tick.
So we have in Pennsylvania ticks, some of those adult blacklegged ticks that transmit Lyme disease, we have about 60% of them that will carry Lyme.
But then also around 14 to 20% of them will also carry anaplasmosis.
So we see some significant levels of these different tickborne illnesses in our tick population, and so we'll test for any of those diseases, even any of the emerging diseases that come out, we'll test for those.
- So has there been a change in the illnesses and diseases that you're seeing in all this time that you've been testing ticks?
Like, what have you seen change over the years?
- Yes, some diseases have emerged.
So Powassan virus has become more common.
One to note is anaplasmosis.
We have seen anaplasmosis increase rapidly over the last few years.
In 2014, we've identified tickborne, not us, but the research world has identified tickborne relapsing fever in New Jersey, of Hunterdon County, and that is a similar infection to Lyme disease.
We've identified other species of the Borrelia bacteria that causes Lyme disease through the upper Midwest, that's Borrelia mayonii.
So we're constantly seeing new species of these bacterial and pathogens that are in these ticks that need to be identified and researched further.
- Wow, so Dr. Lenko, how is Lyme disease diagnosed?
So if someone notices a tick on their body, and then they notice a rash, what happens after that in terms of diagnosis?
- Right, so the diagnosis is, you know, initially if it's just with a tick bite, it's really difficult to diagnose it with a test because what we're really testing for in our patient is a formation of an antibody.
They're mostly antibody-based tests, what we're testing on humans, which is different than what the lab is testing for, the actual tick, where they're looking for the actual bacteria.
So what we're looking at for is the human's response, you know, the antibody response.
So that sometimes takes a few days, often a week or two.
So if you test too early and if you test within the first week or so of removing the tick and you're concerned about it, you often might miss, the test might be falsely negative because it's just too early in the disease to pick up the antibodies.
So what we usually test is there's a first test that we do, which is a primary test, and if that's positive, then they do what's called a confirmatory test with a better test to figure out the antibodies if they're truly present in the body.
So sometimes that takes a couple days, but it's all a blood-based test, that's a blood sample that's provided by the patient.
- So essentially you would need two tests?
- The lab does that automatically.
So if they see the first one come back positive, they automatically will reflex to that to the second test and give that information to you.
And then if it truly is a positive for Lyme disease based on a variety of criteria, then they actually send that information to the health officials as well to track the disease, to track the Lyme disease as well.
- And then Dr. Martin, how would a patient be treated?
- Well, the most common antibiotic we use to treat Lyme disease is called doxycycline.
And you can take it for as short as maybe 10 or 14 days to eliminate the infection.
Although most providers and physicians in the community will typically treat for more like three or four weeks based on older studies.
Doxycycline is, as I said, the most effective antibiotic for this infection.
No other antibiotic's been proven to be better.
Although some other antibiotics can be used.
We don't like to use doxycycline in pregnant women or in young children, although sometimes it can be done under the guidance of some pediatric experts.
- Okay, so would this two-week regimen, would this work to rid your body of Lyme disease, Dr. Martin?
- It does.
The problem is of course not everybody necessarily feels better right away.
I often compare it to strep throat, where if you've ever had strep throat, you have pain and inflammation in your throat and you don't feel well.
And if he goes to the doctor, we can give you penicillin.
And within a few days, as the bacteria dies off, the inflammation dies off, and you tend to feel better.
With Lyme disease, that does not always necessarily happen, and a small percentage of patients may still feel relatively unwell, even after they've finished the antibiotics, suggesting that there may be a disconnect between the killing of the bacteria and the dying off of that inflammation.
Why that is, is not entirely clear.
- So how long might a patient not feel well with Lyme disease, Dr. Lenko?
- It can vary, but oftentimes we see that does take often a few weeks in general, you know, in general, within a few weeks after fully treating with the doxycycline or whatever antibiotic, they are generally feeling better.
Sometimes I do see up to months.
And like Dr. Martin had said, there are a few cases where it can be, you know, a year or two that people continue to feel unwell.
And this is the least understood process that happens after Lyme disease treatment.
But those cases are relatively rare, and most patients feel better within a few weeks.
- Wow.
One to two years, that's a long time.
Would that be considered post-Lyme disease syndrome, Dr. Martin?
- Well, that's sometimes what is called post-Lyme disease syndrome.
This again, as Dr. Lenko pointed out, is fairly poorly understood process, and it can be difficult sometimes to tease out from patients whether or not some of the symptoms they may be experiencing are linked to a previous Lyme infection versus some other disease process, right?
If you feel fatigued, is that because you had a history of Lyme, or is that because you don't get enough sleep at night, or you suffer from depression?
Or something more serious like obstructive sleep apnea, right?
There's all sorts of potential explanations there that kind of cloud the picture.
And sometimes treating these other problems is what patients benefit from the most.
- Right.
So what are the risk factors, Nicole, for contracting Lyme disease, and how can we prevent it?
- So our research has shown that in Pennsylvania, in most areas, you are more likely to be exposed to a tick bite in your own backyard.
50% of our submissions have been people gardening or working in their backyard or playing in their backyard.
So you wanna do some personal prevention and some yard prevention to really help reduce the number of ticks that you have in your yard, and to be aware that tick bite, you'll be at your greatest risk in your backyard because that is usually when you feel most protected is in your own yard.
So spraying your clothes and your skin with some insect repellent, so DEET-based, or your clothing with permethrin-like chemicals.
keeping your trees in your yard trimmed back so you get some direct sunlight on areas, especially areas where children will play.
Ticks do not like areas that are hot and dry.
So also keeping your lawn mowed short helps to keep that area dry and hot.
And ticks will tend to stay on the edges of the woods and underneath the leaf litter where they can go and tucker down and keep cool and moist during the hot summer days.
Also avoiding the edges of the forests when you're in your yard or out recreating.
- Now, these ticks, they don't just stick to deer constantly, I mean, they can...
I mean, they can be anywhere, right, Nicole?
- Yeah, so actually, deer play a role in increasing the number of ticks we see in the population.
But really the disease comes from the white-footed mouse and other small rodents.
They're the reservoir hosts, and they transmit the majority of the diseases that we see in our tick population to the vector of the tick.
And then the tick transmits it to the reservoir host as well.
So really that's where the disease ecology cycle is occurring, with the small rodents.
Deer and other larger mammals will play a role because one tick can feed on an animal and lay up to 2,000 to 4,000 eggs.
And on average, a deer can carry anywhere between 200 and 300 ticks on them at a time.
So they really do play a huge role in increasing the ticks we see in the population, but they don't play a huge role in disease transmission.
- Okay, so what type of rodents?
- The white-footed mouse is gonna be the most common.
They're carriers of Lyme disease, Powassan virus, Babesiosis, anaplasmosis.
- Wow.
So DEET.
You were talking about spraying DEET.
Is DEET a safe repellent, Dr. Martin?
- Yes.
It is certainly.
When used in small quantities, it is perfectly safe and very effective at helping to prevent tick bites.
- Is there an alternative?
'Cause some people are opposed to using chemicals on their body.
- (laughs) There are alternatives.
And if you go to the CDC website, they will list some of those alternatives for you.
I think you heard referenced permethrin, which is also very effective at preventing tick bites.
That's a chemical that you would put on your clothes, or sometimes camping gear, tents, that kind of thing.
If you're gonna be outdoors, that can help prevent tick bites as well.
- So with summer coming and people being outdoors more, should we constantly check ourselves every night just to make sure we don't have any ticks on us, Dr. Lenko?
- Yeah, that's what I was gonna suggest is that the best prevention is to wear long clothing, kind of tuck your pants into your socks.
If you are going outside into the woods, wear long sleeves.
But ticks find a way sometimes to crawl into, you know, under sleeves, et cetera.
So I do recommend every night before bed, for your kids as well, when you're giving them a bath, or recommend they do that themselves when they're older, especially into areas like at the base of the neck, at the ears, that's where I commonly find a tick, or anywhere on the torso, under the arms, places that they can kind of hide.
Yeah, it is recommended.
And to have your partner or somebody in your family check the back of your neck and your hairline if possible, your back and areas that you can't visibly see.
- And pets can transmit Lyme disease as well, Nicole?
- No, they cannot transmit Lyme disease.
So your cats and your dogs will not transmit it to the tick or to you, and people can't transmit Lyme disease to each other.
Only the white-footed mouse and some other small rodents have that ability to transmit the disease.
But dogs can actually get Lyme disease, so they can be exposed to a tick bite and get symptoms similar to what we would see in humans with being lethargic and joint pain.
- And Nicole, do all ticks carry Lyme disease?
- No, not all ticks carry Lyme disease.
All ticks have the capabilities of carrying Lyme disease, I should say that, but only the blacklegged tick, the Ixodes scapularis, has the ability to transmit Lyme disease.
The American dog tick and lone star ticks, they actually have some proteins and other components in their saliva that actually can deactivate the bacteria of Lyme disease before it's transmitted.
So they can carry it, but they're not able to actually transmit it to us.
- So Dr. Lenko, you can be cured of Lyme disease, correct?
- Yes.
Absolutely.
And we treat it relative, unfortunately, commonly in the office.
So we probably see about, maybe in the summer months, probably about a case a month that we either diagnose in the office with a confirmed case in the office.
So we treat it with oral antibiotics, as Dr. Martin said.
And they're very well-tolerated.
You take the full course of the antibiotics and it's treatable, curable.
The thing that does come up sometimes is patients ask, "Well, can I be tested to make sure I don't have it anymore?"
And that's unfortunately not really recommended because you can, if you get tested again soon after having Lyme disease, the antibodies could be from the first infection, and they don't have anything to do with another infection after that.
So you can get infected again, but sometimes it becomes tricky based on the timing of the test that you, if you do it over too soon.
- Okay, and Dr. Martin, since you're a specialist in infectious diseases, is there a vaccine on the horizon for Lyme disease?
- There's a resounding maybe to that answer.
So there have been vaccines which have been developed in the past, one of which was even in use.
It was FDA approved for awhile.
But the manufacturer eventually withdrew it from the market.
There are other companies that have been in the process of developing vaccines for Lyme, some of which look fairly promising.
So it's conceivable that some of those may eventually get to the point to where they are in use again.
- Has Lyme disease become more prevalent over the years, Dr. Martin?
- It has, and there's probably a couple reasons for that.
It may be because of course that the tick itself has spread as deer and mouse populations have changed and as people population have changed and become in more contact with these animals.
Also, we know of course that there's much more testing for Lyme disease than there was say, even 5, 10 years ago.
And when we do more tests, we find more positive results.
- Okay.
Well, that's good to know.
And a lot of people do get Lyme disease, as we said in our open.
And do you foresee that number rising at all, Dr. Martin?
- Yep.
(laughs) We tend to see more contact with more ticks and more tests.
And so I suspect we will see a continued gentle trajectory upwards of cases.
You know, the thing to remember about Lyme disease is that, yes, we have a lot of it in Pennsylvania in particular.
And it can certainly make people feel very sick.
But it is a curable infection.
It is not the chronic problem that some people think it might be.
And that of course gets to a lot of the misinformation that's out there and a lot of misunderstanding about the nature of this infection and what it can do and how it's best treated.
- Okay.
Well, thank you.
This was all very interesting and enlightening.
I appreciate you all joining us to discuss Lyme disease.
Once again, I would like to thank our panelists for participating in this discussion.
For more information and resources on this topic, visit wvia.org/ctd.
I'm Paola Giangiacomo for "Call the Doctor."
Thank you for watching.
(upbeat music) - [Man] Oh, now the mics are open.
- Oh, thank you guys.
That went by really fast.
I appreciate it.
Thanks for joining us.
- Thank you.
- You're welcome.
Have a good evening.
- You guys were great.
- [Woman] Thank you.
I learned a lot.
Lyme Disease: What You Need to Know - Preview
Preview: S33 Ep16 | 30s | Watch Wednesday, May 12th at 7:30pm on WVIA TV (30s)
Clip: S33 Ep16 | 27s | Nicole Chinnici, MS, C.W.F.S. - East Stroudsburg University (27s)
Providing Support for PBS.org
Learn Moreabout PBS online sponsorship
- Science and Nature

Explore scientific discoveries on television's most acclaimed science documentary series.

- Science and Nature

Capturing the splendor of the natural world, from the African plains to the Antarctic ice.












Support for PBS provided by:
Call The Doctor is a local public television program presented by WVIA